January 2, 2010
by meagenda
Dx Revision Watch: Monitoring the progress of the DSM and ICD revision processes
Post #2 Shortlink: http://wp.me/pKrrB-5U
Before using this site please read the Disclaimer Notes

Dx Revision Watch | Monitoring the development of DSM-5, ICD-11, ICD-10-CM
Why another site?
The concept for this site developed out of research and awareness raising undertaken throughout 2009 around the forthcoming revisions of two important international disease classification systems:
The American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM)
The World Health Organization’s International Statistical Classification of Diseases and Related Health Problems (ICD)
How will this site work?
The site will distil information and commentary already published on a companion site around the two revision processes and present this material in a more accessible format. Key information and resources will be added to the Tab Pages as more information becomes available. Updates and new material will be posted on the “Main Page”, which displays the ten most recent postings. Previous posts can be accessed from the monthly archives or from the Post index.
Two new international classification systems by 2015
The next edition of the APA’s Diagnostic and Statistical Manual of Mental Disorders will be DSM-V (DSM-5). The revision of the current version, DSM-IV, began in 1999. DSM-5 is now expected to be published in May 2013 – a year later than had previously been planned.
The revision of the current version of the WHO’s International Statistical Classification of Diseases, ICD-10, and the development of the structure for ICD-11 began in 2007. The WHO anticipates that ICD-11 will be completed by 2015 although targets for population of content for the Alpha Draft have slipped.
Assuming the timelines stay on target, DSM-5 will be published at least two years in advance of ICD-11.
Diagnostic and Statistical Manual of Mental Disorders (DSM)
Commonly referred to as the “Psychiatrist’s Bible”, DSM is used by clinicians in the mental health field for diagnosing mental disorders. It is used by medical insurance companies for reimbursement, in medical practices, clinics and hospitals, by social services agencies, governments, policy makers, courts, forensics, prisons, drug regulation agencies, pharmaceutical companies and researchers.
Diagnostic criteria defined within DSM determine what is considered a mental health disorder and what is not, what medical treatments individuals receive and which treatments health insurers will authorise funding for. The inclusion of a disorder within DSM has revenue implications for pharmaceutical companies seeking licences for new drugs or to expand markets and applications for existing products.
DSM is the primary diagnostic system in the US and is used to a varying extent in other countries. In the UK and some European countries, Chapter V, the Mental and Behavioural Disorders chapter of ICD-10, is also used for diagnosing mental health disorders.
The next edition of DSM will shape international research and influence literature in the fields of psychiatry and psychosomatics for many years to come.
The revision of DSM-IV is being undertaken by a 27 member Task Force and 16 Work Groups. These groups also draw on external advisors who are not being identified. It’s been a controversial process. Some of the most vocal critics have been those who served on Task Force committees for previous revisions, publishing criticism around lack of transparency, potential conflicts of interest from Task Force and Work Group members’ financial links with pharmaceutical companies, lack of dialogue with stakeholder groups, lack of diversity in the make up of the Work Groups, the sketchy and infrequent reports issued by the various Work Groups on their progress.
International Statistical Classification of Diseases (ICD)
The International Statistical Classification of Diseases (ICD) is the international standard diagnostic classification of diseases for use in epidemiology, health management and clinical practice. It is used to classify diseases and other health problems recorded on many types of health and other records, including death certificates and insurance. These records also provide the basis for the compilation of national mortality and morbidity statistics by WHO Member States.
ICD-11 is being revised through a Steering Group and a number of Topic Advisory Groups (TAGs), under Managing Editors, with responsibility for recruiting external peer reviewers and experts for reviewing proposals and advising on content. The WHO is promoting the development of ICD-11 as an open and transparent process.
Drafting is being carried out via a collaborative authoring platform – the iCAT, with a second, publicly viewable platform known as the Alpha Browser. Key documentation, style guides, models for the population of content and information on the structure of ICD-11 is being posted on a dedicated, public domain website.
According to the ICD-11 Timeline, the Beta draft is currently scheduled for release in May 2012.
When are the first drafts of DSM-5 and ICD-11 due?
The APA published its first draft proposals for DSM-5 diagnostic categories on a new website, on February 10, 2010.
APA webpages for DSM-5 development: DSM-5 Development
Information on DSM-5 draft criteria for the Somatic Symptom Disorders as they stood at February 2010 was published on this page:
DSM-5 draft and stakeholder feedback process
The first public review ran from February 10 to April, 20, 2010
The second public review ran from May 4 to July 15, 2011
The third public review is expected to be released in May 2012, at the latest
The ICD-11 Alpha Draft is currently timelined for May 2010.
The “harmonization” of DSM-5 and ICD-11
The APA participates with the WHO in the International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders and the DSM-ICD Harmonization Coordination Group.
There is already a degree of correspondence between DSM-IV categories and Chapter V of ICD-10. For the next editions, the APA and the WHO have committed as far as possible:
To facilitate the achievement of the highest possible extent of uniformity and harmonization between ICD-11 mental and behavioural disorders and DSM-V disorders and their diagnostic criteria.
with the objective that
The WHO and APA should make all attempts to ensure that in their core versions, the category names, glossary descriptions and criteria are identical for ICD and DSM.
The WHO acknowledges that there may be areas where congruency may not be achievable.
Will ICD-11 be implemented worldwide from 2015?
No. Several countries have developed their own “Clinical Modifications (CM)” of ICD. Canada, for example, uses an adaptation called ICD-10-CA, with a version published for 2009. Germany uses a version called ICD-10-GM. Australia and Thailand also use country specific adaptations of ICD-10.
The US currently uses a CM version of ICD-9 (long since retired by the WHO and replaced with ICD-10). But instead of moving onto ICD-11, once this is completed, the US will be implementing a Clinical Modification of ICD-10 called ICD-10-CM, on October 1, 2013.
There are disparities between some of the proposed codings for the forthcoming US Clinical Modification, ICD-10-CM and those in ICD-10: for example, chapter placement and codings for Postviral fatigue syndrome, (Benign) myalgic encephalomyelitis and Chronic fatigue syndrome in ICD-10 differs from the current proposals for ICD-10-CM.
Are the two revisions on schedule?
The original dissemination date for ICD-11 had been 2012, with the timelines for revision of both systems running more or less in parallel. The dissemination date for ICD-11 was later extended to 2014, then 2015, but work on the Alpha Draft is behind schedule.
The timeline for DSM-5 has also slipped. APA originally planned to publish DSM-5 in May 2012. But in a press release issued on 10 December 2009, APA announced that it was postponing publication for a further year, until May 2013, “to allow more time for public review, field trials and revisions.”
The press release also stated:
• The extension will also permit the DSM-5 to better link with the U.S. implementation of the ICD-10-CM codes for all Medicare/Medicaid claims reporting, scheduled for October 1, 2013.
• The ICD-10-CM includes disorder names, logical groupings of disorders and code numbers but not explicit diagnostic criteria. The APA has already worked with CMS and CDC to develop a common structure for the currently in-use DSM-IV and the mental disorders section of the ICD-10-CM.
• APA will continue to work with the WHO to harmonize the DSM-5 with the mental and behavioral disorders section of the ICD-11. Given the timing of the release of both DSM-5 and ICD-11 in relation to the ICD-10-CM, the APA will also work with the CDC and CMS to propose a structure for the U.S. ICD-10 CM that is reflective of the DSM-5 and ICD-11 harmonization efforts. This will be done prior to the time when the ICD-10-CM revisions are “frozen” for CMS and insurance companies to prepare for the October 1, 2013, adoption.
With the three systems: DSM-5 (ETA now May 2013), ICD-10-CM (subject to a partial code freeze on October 1, 2010 until 2014), with an ETA for implementation on October 1, 2013) and ICD-11 (dissemination in 2015+ but Alpha behind schedule) set to become more closely aligned, the proposed structure of ICD-11 may have implications for US patient populations, even though the US might not anticipate moving on to ICD-11 (or a CM of ICD-11) for many years (one source estimates 2018+).
What will be the focus for this site?
• Monitoring the progress of the revision of ICD-10 Chapter VI: Diseases of the nervous system (the Neurological chapter) with specific reference to the classifications coded in ICD-10 Volume 1: The Tabular list at G93.3: Postviral fatigue syndrome; (Benign) myalgic encephalomyelitis, and indexed in Volume 3: The Alphabetical Index at G93.3: Chronic fatigue syndrome.
• Monitoring the population of content to be included in ICD-11 for these three entities.
• Monitoring the progress of the revision of the DSM category section currently called Somatoform Disorders being undertaken by the DSM-5 Somatic Symptom Disorders Work Group.
• Monitoring the progress of the revision of the corresponding Somatoform Disorders section in ICD-10 Chapter 5 (Mental and Behavioural Disorders) with specific reference to the categories currently classified under Somatoform Disorders at F45 – F48.0.
• Monitoring any “harmonization” of the corresponding category sections in DSM-5 and ICD-11 currently called Somatoform Disorders.
Issues for ICD-11
Content in ICD-11 will be populated for thirteen parameters, in accordance with the ICD-11 Content Model Style Guide. There is the potential for considerably more content to be included for diseases, disorders and syndromes in ICD-11 than appears in ICD-10, including Definition, Inclusions and Causal Mechanisms.
It is not known how much additional information might be included in ICD-11 for the three terms currently classified at, or indexed to, G93.3. Content will need to be monitored, as it is generated, as will any changes to the hierarchy between these three terms, as will specification of the relationships between the three terms.
Issues for DSM-5
Chronic fatigue syndrome is not categorized within DSM-IV and neither is Neurasthenia. In ICD-10, Neurasthenia is classified in Chapter V at F48.0 (for the forthcoming ICD-10-CM, in Chapter 5 at F48.8).
Professionals in the field, interest groups and the media have been voicing concerns for several years that the introduction of new disorders and the lowering of thresholds for existing criteria for some categories would bring many more patients under a mental health diagnosis.
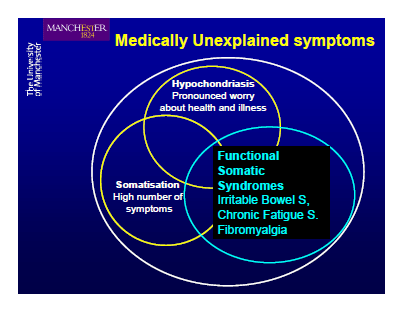
But if the most recently published proposals by the Somatic Symptom Disorders Work Group were to be approved there may be medical, social and economic implications to the detriment of all patient populations – but especially those bundled by many psychiatrists under the so-called Functional Somatic Syndromes (FSS) and Medically Unexplained Syndromes (MUS) umbrellas, under which they include ME, CFS, FM, IBS, CI, CS, chronic Lyme disease, GWS and some others disorders and conditions.
In a presentation to The Academy of Psychosomatic Medicine, in November 2009, Somatic Symptom Disorders Work Group Chair, Joel E Dimsdale, reported that the group was considering a proposal for a new category (then, tentatively entitled, “Somatic Symptom Disorder”) to replace the DSM-IV Somatoform and related disorders which would include somatoform disorders (somatization disorder, hypochondriasis, pain disorder, and undifferentiated somatoform disorder), factitious disorders, and psychological factors affecting medical condition. The group was exploring the potential for de-emphasizing “medically unexplained symptoms”, as the term was considered “divisive”, fostered “mind-body dualism” and contributed to “doctor-patient antagonism.”
See Post #8, January 12, 2010: APM 2009 Annual Meeting Workshop: DSM-V for Psychosomatic Medicine: Current Progress and Controversies

Image source: Academy of Psychosomatic Medicine, Nevada, November ‘09 Annual Meeting slide presentation, Francis Creed, MD, FRCP: Can We Now Explain Medically Unexplained Symptoms?
In the June 2009 Journal of Psychosomatic Research Editorial “The proposed diagnosis of somatic symptom disorders in DSM-V to replace somatoform disorders in DSM-IV – a preliminary report”, which expanded on the brief April 2009 Work Group progress report published on the APA’s website, Work Group Chair, Joel E Dimsdale, and fellow Work Group member, Francis Creed, reported that by doing away with the “controversial concept of medically unexplained”, their proposed classification might diminish the “dichotomy, inherent in the ‘Somatoform’ section of DSM-IV, between disorders based on medically unexplained symptoms and patients with organic disease.”
The conceptual framework the Work Group were proposing, at that point:
“…will allow a diagnosis of somatic symptom disorder in addition to a general medical condition, whether the latter is a well-recognized organic disease or a functional somatic syndrome such as irritable bowel syndrome or chronic fatigue syndrome.”
The most recent version of the Somatic Symptom Disorders Disorders description proposals document states:
“These disorders typically present first in non-psychiatric settings and somatic symptom disorders can accompany diverse general medical as well as psychiatric diagnoses. Having somatic symptoms of unclear etiology is not in itself sufficient to make this diagnosis. Some patients, for instance with irritable bowel syndrome or fibromyalgia would not necessarily qualify for a somatic symptom disorder diagnosis. Conversely, having somatic symptoms of an established disorder (e.g. diabetes) does not exclude these diagnoses if the criteria are otherwise met.
Javier Escobar, MD, Director of the University of Medicine and Dentistry of New Jersey (UMDNJ) – Robert Wood Johnson Medical School (RWJMS) Medically Unexplained Physical Symptoms (MUPS) Research Center, which has been supported with over $4M in funding by the US National Institute of Mental Health (NIMH), is a member of the DSM-5 Task Force. Dr Escobar serves as a Task Force liaison to the Somatic Symptom Disorders Work Group and is said to work closely with this group.
In the August 2008 Special Report for Psychiatric Times: “Unexplained Physical Symptoms What’s a Psychiatrist to Do?” co-authors, Escobar and Marin wrote:
“…Perhaps as a corollary of turf issues, general medicine and medical specialties started carving these syndromes with their own tools. The resulting list of ‘medicalized’, specialty-driven labels that continues to expand includes fibromyalgia, chronic fatigue syndome, multiple chemical sensitivity, and many others.
“…These labels fall under the general category of functional somatic syndromes and seem more acceptable to patients because they may be perceived as less stigmatizing than psychiatric ones. However, using DSM criteria, virtually all these functional syndromes would fall into the somatoform disorders category given their phenomenology, unknown physical causes, absence of reliable markers, and the frequent coexistence of somatic and psychiatric symptoms.”
In Table 1, under the heading “Functional Somatic Syndromes (FSS)” Escobar and Marin list:
Irritable bowel syndrome, Chronic fatigue syndrome, Fibromyalgia, Multiple chemical sensitivity, Nonspecific chest pain, Premenstrual disorder, Non-ulcer dyspepsia, Repetitive strain injury, Tension headache, Temporomandibular joint disorder, Atypical facial pain, Hyperventilation syndrome, Globus syndrome, Sick building syndrome, Chronic pelvic pain, Chronic whiplash syndrome, Chronic Lyme disease, Silicone breast implant effects, Candidiasis hypersensivity, Food allergy, Gulf War syndrome, Mitral valve prolapse, Hypoglycemia, Chronic low back pain, Dizziness, Interstitial cystitis, Tinnitus, Pseudoseizures, Insomnia, Systemic yeast infection, Total allergy syndrome
The Somatic Symptom Disorders Work Group proposes redefining the categories in the Somatoform Disorders section of DSM-IV to legitimize the application of an additional “bolt-on” diagnosis of a “somatic symptom disorder” for all medical diseases, whether “established general medical conditions or disorders”, like diabetes or angina, or conditions presenting with “somatic symptoms of unclear etiology”, if the criteria are otherwise met.
The criteria as they currently stand are vague, highly subjective and difficult to measure. ME, CFS, FM, IBS, CI, CS, chronic Lyme disease and Gulf War illness may be particularly vulnerable to being caught by these criteria.
These radical proposals for rebranding the Somatoform Disorders categories as Somatic Symptom Disorders and combining a number of existing, little-used categories under the proposed portmanteau term, Complex Somatic Symptom Disorder (CSSD), and the more recently proposed, Simple Somatic Symptom Disorder (SSSD), have the potential for bringing many thousands more patients under a mental health banner.
The potential for expanding markets for psychiatric services, antidepressants and behavioural therapies, like CBT, for the “modification of dysfunctional and maladaptive beliefs about symptoms and disease, and behavioral techniques to alter illness and sick role behaviors” for all patients with somatic symptoms, if the clinician considers that the patient’s response (or in the case of a child, a parent’s response) to bodily symptoms and concerns about health are “excessive”, or the perception of their level of disability “disproportionate”, or their coping styles, “maladaptive.”
Application of these vague, highly subjective and difficult to measure criteria may have considerable implications for the diagnoses assigned to patients, the provision of social care, the payment of employment, medical and disability insurance and the length of time for which insurers are prepared to pay out.
The misapplication of a diagnosis of Complex Somatic Symptom Disorder (CSSD), may limit the types of treatment, medical investigations and testing that clinicians are prepared to consider and for which insurers are prepared to fund.
These proposals could potentially result in misdiagnosis of a mental health disorder, misapplication of an additional “bolt-on” diagnosis of a mental health disorder, missed diagnoses through failure to investigate new or worsening symptoms, or in iatrogenic disease from psychotropic drugs.
Families caring for children and young people with any long-term illness may be at increased risk of wrongful accusation of “over-involvement” or “excessive” concern for a child’s symptomatology or of encouraging maintenance of “sick role behaviour” in an ill child or adolescent.
Acording to Task Force Chair, Dr. David Kupfer, MD, the specific diagnostic categories that received the most feedback during the second public review and feedback exercise were sexual and gender identity disorders, followed closely by somatic symptom disorders and anxiety disorders.
image credit | belgianchocolate | creative commons
Dx Revision Watch is maintained by Suzy Chapman. To contact please use the Contact page.
A version of this posting is also published on the About Page