April 28, 2017
by admindxrw
A copy of this post in PDF format is available here

1 Why is this proposal for ICD-11 so important?
1.1 The International Statistical Classification of Diseases and Related Health Problems (ICD) is the standard diagnostic classification of diseases for use in epidemiology, health management, clinical practice and reimbursement. ICD-10 has been translated into 43 languages and is used by WHO member states in over 100 countries.
It provides a common language for reporting and monitoring the incidence and prevalence of diseases and other health problems. This allows for global comparison and data sharing in a consistent, standardized way between hospitals, regions and countries and over periods of time.
ICD is used to report and summarize an episode of care after the event. Data recorded on many types of medical information and other records, including death certificates, provides the basis for analyses of national mortality and morbidity statistics by WHO member states, which are used to inform decision-makers and commissioners and to monitor health related spending.
Users include physicians, nurses, allied health care providers, researchers, health information managers and technology workers, coders, policy-makers and insurers [1].
ICD-11 is an electronic product designed to be used in computerized health information systems and will link to other globally used clinical terminology systems, like SNOMED CT.
Inappropriate classification of the G93.3 “legacy” categories for ICD-11 will negatively influence perceptions of the disease and the clinical care that patients receive throughout the world ‒ with implications for service commissioning, the types of medical investigations and treatments that clinicians are prepared to consider and medical insurers prepared to fund, the provision of welfare benefits, social care, disability adaptations, education and workplace accommodations.
It is crucial that international organizations, their clinical and research allies and patient and advocate stakeholders take some time to review our proposal, register with the Beta draft and submit a considered response. Over 45 stakeholder organizations have already commented in support.
1.2 After four years of uncertainty, it’s important that the G93.3 “legacy” terms are included and appropriately classified for the initial 2018 release of ICD-11
Although revision of ICD-10 has been underway since 2007, the work group with responsibility for the G93.3 categories has yet to reach consensus over how these terms should be classified for the new edition. Since early 2013, there have been no proposals in the public version of the ICD-11 Beta draft for stakeholders to review, input into or comment on.
The terms were finally restored to the Beta draft on March 26, but with this caveat: “While the optimal place in the classification is still being identified, the entity has been put back to its original place in ICD.”
Evidently, the work group has not yet reached consensus (or if it has, has not reached consensus with the WHO classification experts and Joint Task Force, to which it reports).
1.3 Why is the timing so critical?
In order to present an initial version of ICD-11 to the World Health Assembly in May 2018, the classification will need to be finalized by the end of this year. For proposals to be considered for inclusion in the 2018 release, they were required to be submitted by a March 30 deadline.
That leaves us with this situation:
- virtually no information about what the work group might be considering;
- having missed the March 30 deadline, no indication of whether any proposals that might be released by the work group between now and the end of the year would be included in the initial 2018 release or rolled forward for consideration for inclusion in the 2019 release;
- if no consensus has been reached before the end of the year, whether the classification would go forward with the “placeholder” listing or whether the terms would be omitted from the initial 2018 release.
Given the uncertainties, it was crucial we submit an alternative option. Stakeholders need to submit comments as soon as possible as it’s not clear whether there is a cut off point for consideration of comments on proposals that met the March 30 deadline.
1.4 Classification is important for protection against misdiagnosis and medical mismanagement
Prior to July 2015 (in the case of SNOMED CT) and prior to April 2016 (in the case of the UK Read Codes CTV3 primary care terminology system) both terminology systems had CFS, ME and their synonym terms dual classified under mental health disorders.
The WHO’s unmodified ICD-10 does not include CFS in the Tabular List, only in the Index. But in the Tabular List, ICD-10 includes several other coded terms which have been misapplied to CFS and ME patients, notably, the various ICD-10 Somatoform disorders categories and Fatigue syndrome, which is coded to Neurasthenia.
Misapplication of these codes has been used to deny patients access to appropriate medical care, to secondary referrals, investigations, emergency treatment, benefits, social care and disability services and in some cases, used to section patients for psychiatric treatment against their will.
Families are still being referred to social services and child protection agencies. Children and young people continue to be removed from parental care because an existing diagnosis of CFS or ME has been contested or because they have been wrongly diagnosed with “Pervasive refusal syndrome” or as “school refusers,” or their parents accused of “Factitious disorder imposed on another.”
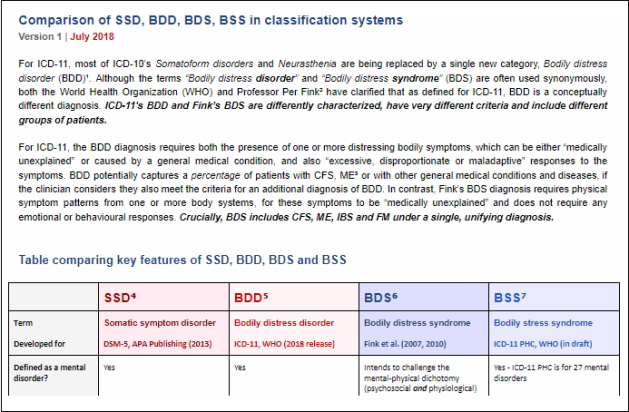
The Somatoform disorders, Neurasthenia and Fatigue syndrome are being replaced for ICD-11 with a new, single “Bodily distress disorder (BDD)” category which is close to the DSM-5 “Somatic symptom disorder (SSD).” BDD poses the same threat to CFS and ME patients as DSM-5’s SSD.
The Netherlands and Germany have witnessed the roll-out of guidelines and services for “MUS” and for “functional somatic syndromes.”
Already in use in Denmark, in clinics and research, Per Fink seeks to colonize Europe with the “Bodily distress syndrome” diagnostic construct, which subsumes and replaces CFS, ME, IBS and FM.
Last year, the Ministry of Science and Research, Hamburg, Germany, provided funding for EURONET-SOMA (European Network to improve diagnosis, treatment and health care for patients with persistent somatic symptoms) comprising a panel of 29 researchers from Denmark, the Netherlands, Sweden, Norway, Latvia, Belgium, United Kingdom, Germany and Russia, to develop a joint research agenda and work towards a common understanding of the terminology, conceptualization and management of “persistent somatic symptoms” and for interdisciplinary agreement on a consistent diagnostic classification.
In the UK, “Medically unexplained symptoms (MUS)” and “Persistent physical symptoms (PPS)” services are proliferating. Funding is being made available for integrated IAPT (Improving Access to Psychological Therapies) services delivering CBT and other therapies for “MUS”; in some cases, bids are being invited specifically for developing IAPT CBT or CBT/GET for CFS patients. One NHS Trust had invited Per Fink and his colleagues over to the UK to train up local GPs in the TERM model.
In at least one part of the country, a specialised CFS service has been decommissioned in order to save money and put out to tender for a combined IAPT type service for CFS and chronic pain.
A new “Joint Commissioning Panel for Mental Health Guidance for commissioners of services for people with medically unexplained symptoms” guideline was published in February, in which CFS and ME are included as “functional somatic syndromes” [2].
The push to commission “MUS” services is relentless. UK patients have reported having their CFS, ME diagnoses challenged by their practitioners and re-diagnosed with “MUS” or with a mental health disorder.
Patients need protection: the G93.3 “legacy” terms must be appropriately classified for ICD-11; safeguarded with reciprocal exclusions for “Fatigue” and “Bodily distress disorder” and not secondary parented under inappropriate chapters or parent classes.
Extract from ICD-11 Beta Proposal Q & A Suzy Chapman, April 2017 version 2
Key links
For a summary of our proposal and links for submitting comment via the Beta draft see: A proposal for the ICD-10 G93.3 legacy terms for ICD-11: Part Two
A PDF Q & A for our proposal can be downloaded here
A copy of this post in PDF format is available here