October 23, 2011
by meagenda
Open Letter and Petition to DSM-5 Task Force by Society for Humanistic Psychology (Division 32 of the American Psychological Association)
Post #107 Shortlink: http://wp.me/pKrrB-1jI
Update @ January 11, 2012: The third and final draft of proposals for changes to DSM-IV categories and criteria is delayed because field trials and evaluations are running behind schedule and extended to March. The final draft is now expected to be released for public review and comment, “no later than May 2012”, according to DSM-5 Task Force Vice-chair, Darrel Regier, MD [1].
Third review of DSM-5 draft proposals on the horizon
This time last year, folk were mailing me saying – I don’t know why you bother continuing to monitor DSM-5 and ICD-11, XMRV is going to render the DSM-5 proposals meaningless.
Well that was then, and this is now. And in a couple of months’ time we’ll be anticipating the third and final public review and feedback on the APA’s draft proposals for changes to categories and criteria for the revision of DSM-IV.
During the first stakeholder feedback exercise, over 8,600 comments rolled in; during the second comment period (which was extended by an additional four weeks), the Task Force and work groups received over 2000 submissions.
According to the current DSM-5 Timeline:
“September-November 2011: Work groups will be provided with results from both field trials and will update their draft criteria as needed. Field trial results and revised proposals will be reviewed at the November Task Force meeting.
“January-February 2012: Revised draft diagnostic criteria will be posted on http://www.dsm5.org and open to a third public feedback period for two months. Feedback will be shared directly with work group members, and further edits to proposals will be made as needed.” [1]
According to the DSM-5 Development home page:
“…Following analysis of field trial results, we will revise the proposed criteria as needed and, after appropriate review and approval, we will post these changes on this Web site. At that time, we will again open the site to a third round of comments from visitors, which will be systematically reviewed by each of the work groups for consideration of additional changes. Thus, the current commenting period is not the final opportunity for you to submit feedback, and subsequent revisions to DSM-5 proposals will be jointly informed by field trial findings as well as public commentary…” [2]
Assuming the APA’s schedule remains on target, US and international patient organizations and advocates need to start preparing well in advance of the New Year for how best to engage our own medical and allied professionals in this process and encourage their input.
As soon as DSM-5 Draft 3 is posted on the DSM-5 Development site, I shall put out alerts on my websites, via Co-Cure and on other platforms and I shall be contacting UK patient organizations, as I have done for the previous two public review exercises.
But I hope that other advocates and groups, in the US and internationally, will work to take this forward and ensure that as many international patient organizations, ME and CFS clinicians and researchers, like those who collaborated on the new ME International Consensus Criteria, allied health professionals, medical lawyers, social workers and other end uses of the DSM are made aware of the proposals of the “Somatic Symptom Disorders” Work Group and the implications for ME, CFS, FM, IBS, CI, CS and GWS patient groups, and encouraged to submit comments as professional stakeholders.
Open Letter and Petition to DSM-5 Task Force
Today I was alerted to an Open Letter and Petition sponsored by the Society for Humanistic Psychology, Division 32 of the American Psychological Association, in alliance with the Society for Community Research and Action: Division of Community Psychology (Division 27 of APA) and the Society for Group Psychology and Psychotherapy (Division 49 of APA) [3]. (No press release, but I’ll update if one is issued.)
These American Psychological Association Divisions are inviting mental health professionals and mental health organizations to sign up in support of an open letter to the American Psychiatric Association’s DSM-5 Task Force.
Their response to DSM-5 structure and proposals may be of interest to psychiatrists and psychologists affiliated to, or on the boards of our own ME and CFS patient organizations.
The Open Letter to the DSM-5 Task Force can be read here and a copy is appended:
http://www.ipetitions.com/petition/dsm5/
Under the subheading “New Emphasis on Medico-Physiological Theory”, the Open Letter sponsors comment on some aspects of the DSM-5 proposals for the “Somatic Symptom Disorders” categories. The Open Letter also supports concerns set out within the formal response to DSM-5 draft proposals submitted by the British Psychological Society, earlier this year, and more recent concerns published by the American Counseling Association.
A couple of points: both the American Psychological Association, three of whose Divisions are sponsors of this Open Letter, and the American Psychiatric Association use the acronym “APA”. It is the American Psychiatric Association’s DSM-5 Task Force that is developing the DSM-5.
Secondly, although the first release of the DSM-5 draft proposals did have the diagnosis “Factitious Disorder” placed under “Somatic Symptom Disorders (SSDs)”, the most recent (May 2011) DSM-5 draft proposes placing “Factitious Disorder” under the diagnostic chapter “Other Disorders”, not within the SSDs, as the Open Letter, below, states [4], [5].
Suzy Chapman
[1] DSM-5 Development Timeline: http://www.dsm5.org/about/Pages/Timeline.aspx
[2] DSM Development website: http://www.dsm5.org/Pages/Default.aspx
[3] Society for Humanistic Psychology: http://www.apadivisions.org/division-32/index.aspx
[4] DSM-5 Draft Proposals, Somatic Symptom Disorders: http://www.dsm5.org/proposedrevision/Pages/SomaticSymptomDisorders.aspx
[5] DSM-5 Draft Proposals, Other Disorders: http://www.dsm5.org/proposedrevision/Pages/OtherDisorders.aspx
The Open Letter and Petition can be read here: http://www.ipetitions.com/petition/dsm5/
There’s also a copy on the blog of Society for Humanistic Psychology
Sponsor
Society for Humanistic Psychology, Division 32 of the American Psychological Association, in alliance with Society for Community Research and Action: Division of Community Psychology (Division 27 of APA) and Society for Group Psychology and Psychotherapy (Division 49 of APA). We invite mental health professionals and mental health organizations to sign on in support of this petition to the DSM5 Task Force of the American Psychiatric Association
To the DSM-5 Task Force and the American Psychiatric Association:
As you are aware, the DSM is a central component of the research, education, and practice of most licensed psychologists in the United States. Psychologists are not only consumers and utilizers of the manual, but we are also producers of seminal research on DSM-defined disorder categories and their empirical correlates. Practicing psychologists in both private and public service utilize the DSM to conceptualize, communicate, and support their clinical work.
For these reasons, we believe that the development and revision of DSM diagnoses should include the contribution of psychologists, not only as select individuals on a committee, but as a professional community. We have therefore decided to offer the below response to DSM-5 development. This document was composed in recognition of, and with sensitivity to, the longstanding and congenial relationship between American psychologists and our psychiatrist colleagues.
Overview
Though we admire various efforts of the DSM-5 Task Force, especially efforts to update the manual according to new empirical research, we have substantial reservations about a number of the proposed changes that are presented on www.dsm5.org. As we will detail below, we are concerned about the lowering of diagnostic thresholds for multiple disorder categories, about the introduction of disorders that may lead to inappropriate medical treatment of vulnerable populations, and about specific proposals that appear to lack empirical grounding. In addition, we question proposed changes to the definition(s) of mental disorder that deemphasize sociocultural variation while placing more emphasis on biological theory. In light of the growing empirical evidence that neurobiology does not fully account for the emergence of mental distress, as well as new longitudinal studies revealing long-term hazards of standard neurobiological (psychotropic) treatment, we believe that these changes pose substantial risks to patients/clients, practitioners, and the mental health professions in general.
Given the changes currently taking place in the profession and science of psychiatry, as well as the developing empirical landscape from which psychiatric knowledge is drawn, we believe that it is important to make our opinions known at this particular historical moment. As stated at the conclusion of this letter, we believe that it is time for psychiatry and psychology collaboratively to explore the possibility of developing an alternative approach to the conceptualization of emotional distress. We believe that the risks posed by DSM-5, as outlined below, only highlight the need for a descriptive and empirical approach that is unencumbered by previous deductive and theoretical models.
In more detail, our response to DSM-5 is as follows:
Advances Made by the DSM-5 Task Force
We applaud certain efforts of the DSM-5 Task Force, most notably efforts to resolve the widening gap between the current manual and the growing body of scientific knowledge on psychological distress. In particular, we appreciate the efforts of the Task Force to address limitations to the validity of the current categorical system, including the high rates of comorbidity and Not Otherwise Specified (NOS) diagnoses, as well as the taxonomic failure to establish ‘zones of rarity’ between purported disorder entities (Kendell & Jablensky, 2003). We agree with the APA/DSM-5 Task Force statement that, from a systemic perspective,
The DSM-III categorical diagnoses with operational criteria were a major advance for our field, but they are now holding us back because the system has not kept up with current thinking. Clinicians complain that the current DSM-IV system poorly reflects the clinical realities of their patients. Researchers are skeptical that the existing DSM categories represent a valid basis for scientific investigations, and accumulating evidence supports this skepticism. (Schatzberg, Scully, Kupfer, & Regier, 2009)
As researchers and clinicians, we appreciate the attempt to address these problems. However, we have serious reservations about the proposed means for doing so. Again, we are concerned about the potential consequences of the new manual for patients and consumers; for psychiatrists, psychologists, and other practitioners; and for forensics, health insurance practice, and public policy. Our specific reservations are as follows:
Lowering of Diagnostic Thresholds
The proposal to lower diagnostic thresholds is scientifically premature and holds numerous risks. Diagnostic sensitivity is particularly important given the established limitations and side-effects of popular antipsychotic medications. Increasing the number of people who qualify for a diagnosis may lead to excessive medicalization and stigmatization of transitive, even normative distress. As suggested by the Chair of DSM-IV Task Force Allen Frances (2010), among others, the lowering of diagnostic thresholds poses the epidemiological risk of triggering false-positive epidemics.
We are particularly concerned about:
• “Attenuated Psychosis Syndrome,” which describes experiences common in the general population, and which was developed from a “risk” concept with strikingly low predictive validity for conversion to full psychosis.
• The proposed removal of Major Depressive Disorder’s bereavement exclusion, which currently prevents the pathologization of grief, a normal life process.
• The reduction in the number of criteria necessary for the diagnosis of Attention Deficit Disorder, a diagnosis that is already subject to epidemiological inflation.
• The reduction in symptomatic duration and the number of necessary criteria for the diagnosis of Generalized Anxiety Disorder.
Though we also have faith in the perspicacity of clinicians, we believe that expertise in clinical decision-making is not ubiquitous amongst practitioners and, more importantly, cannot prevent epidemiological trends that arise from societal and institutional processes. We believe that the protection of society, including the prevention of false epidemics, should be prioritized above nomenclatural exploration.
Vulnerable Populations
We are also gravely concerned about the introduction of disorder categories that risk misuse in particularly vulnerable populations. For example, Mild Neurocognitive Disorder might be diagnosed in elderly with expected cognitive decline, especially in memory functions. Additionally, children and adolescents will be particularly susceptible to receiving a diagnosis of Disruptive Mood Dysregulation Disorder or Attenuated Psychosis Syndrome. Neither of these newly proposed disorders have a solid basis in the clinical research literature, and both may result in treatment with neuroleptics, which, as growing evidence suggests, have particularly dangerous side-effects (see below)—as well as a history of inappropriate prescriptions to vulnerable populations, such as children and the elderly
Sociocultural Variation
The DSM-5 has proposed to change the Definition of a Mental Disorder such that DSM-IV’s Feature E: “Neither deviant behavior (e.g., political, religious, or sexual) nor conflicts that are primarily between the individual and society are mental disorders unless the deviance or conflict is a symptom of a dysfunction in the individual,” will instead read “[A mental disorder is a behavioral or psychological syndrome or pattern] [t]hat is not primarily a result of social deviance or conflicts with society.” The latter version fails to explicitly state that deviant behavior and primary conflicts between the individual and society are not mental disorders. Instead, the new proposal focuses on whether mental disorder is a “result” of deviance/social conflicts. Taken literally, DSM-5’s version suggests that mental disorder may be the result of these factors so long as they are not “primarily” the cause. In other words, this change will require the clinician to draw on subjective etiological theory to make a judgment about the cause of presenting problems. It will further require the clinician to make a hierarchical decision about the primacy of these causal factors, which will then (partially) determine whether mental disorder is said to be present. Given lack of consensus as to the “primary” causes of mental distress, this proposed change may result in the labeling of sociopolitical deviance as mental disorder.
Revisions to Existing Disorder Groupings
Several new proposals with little empirical basis also warrant hesitation:
• As mentioned above, Attenuated Psychosis Syndrome and Disruptive Mood Dysregulation Disorder (DMDD) have questionable diagnostic validity, and the research on these purported disorders is relatively recent and sparse.
• The proposed overhaul of the Personality Disorders is perplexing. It appears to be a complex and idiosyncratic combined categorical-dimensional system that is only loosely based on extant scientific research. It is particularly concerning that a member of the Personality Disorders Workgroup has publicly described the proposals as “a disappointing and confusing mixture of innovation and preservation of the status quo that is inconsistent, lacks coherence, is impractical, and, in places, is incompatible with empirical facts” (Livesley, 2010), and that, similarly, Chair of DSM-III Task Force Robert Spitzer has stated that, of all of the problematic proposals, “Probably the most problematic is the revision of personality disorders, where they’ve made major changes; and the changes are not all supported by any empirical basis.”
• The Conditions Proposed by Outside Sources that are under consideration for DSM-5 contain several unsubstantiated and questionable disorder categories. For example, “Apathy Syndrome,” “Internet Addiction Disorder,” and “Parental Alienation Syndrome” have virtually no basis in the empirical literature.
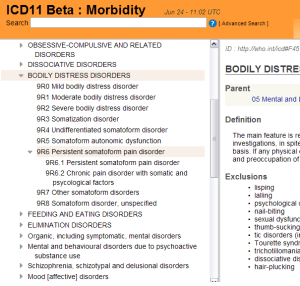
New Emphasis on Medico-Physiological Theory
Advances in neuroscience, genetics, and psychophysiology have greatly enhanced our understanding of psychological distress. The neurobiological revolution has been incredibly useful in conceptualizing the conditions with which we work. Yet, even after “the decade of the brain,” not one biological marker (“biomarker”) can reliably substantiate a DSM diagnostic category. In addition, empirical studies of etiology are often inconclusive, at best pointing to a diathesis-stress model with multiple (and multifactorial) determinants and correlates. Despite this fact, proposed changes to certain DSM-5 disorder categories and to the general definition of mental disorder subtly accentuate biological theory. In the absence of compelling evidence, we are concerned that these reconceptualizations of mental disorder as primarily medical phenomena may have scientific, socioeconomic, and forensic consequences. New emphasis on biological theory can be found in the following DSM-5 proposals:
• The first of DSM-5’s proposed revisions to the Definition of a Mental Disorder transforms DSM-IV’s versatile Criterion D: “A manifestation of a behavioral, psychological, or biological dysfunction in the individual” into a newly collapsed Criterion B: [A behavioral or psychological syndrome] “That reflects an underlying psychobiological dysfunction.” The new definition states that all mental disorders represent underlying biological dysfunction. We believe that there is insufficient empirical evidence for this claim.
• The change in Criterion H under “Other Considerations” for the Definition of a Mental Disorder adds a comparison between medical disorders and mental disorders with no discussion of the differences between the two. Specifically, the qualifying phrase “No definition adequately specifies precise boundaries for the concept of ‘mental disorder” was changed to “No definition perfectly specifies precise boundaries for the concept of either ’medical disorder’ or ‘mental/psychiatric disorder’.” This effectively transforms a statement meant to clarify the conceptual limitations of mental disorder into a statement equating medical and mental phenomena.
• We are puzzled by the proposals to “De-emphasize medically unexplained symptoms” in Somatic Symptom Disorders (SSDs) and to reclassify Factitious Disorder as an SSD. The SSD Workgroup explains: “…because of the implicit mind-body dualism and the unreliability of assessments of ‘medically unexplained symptoms,’ these symptoms are no longer emphasized as core features of many of these disorders.” We do not agree that hypothesizing a medical explanation for these symptoms will resolve the philosophical problem of Cartesian dualism inherent in the concept of “mental illness.” Further, merging the medico-physical with the psychological eradicates the conceptual and historical basis for somatoform phenomena, which are by definition somatic symptoms that are not traceable to known medical conditions. Though such a redefinition may appear to lend these symptoms a solid medico-physiological foundation, we believe that the lack of empirical evidence for this foundation may lead to practitioner confusion, as might the stated comparison between these disorders and research on cancer, cardiovascular, and respiratory diseases.
• The proposed reclassification of Attention Deficit/Hyperactivity Disorder (ADHD) from Disorders Usually First Diagnosed in Infancy, Childhood, or Adolescence to the new grouping “Neurodevelopmental Disorders” seems to suggests that that ADHD has a definitive neurological basis. This change, in combination with the proposal to lower the diagnostic threshold for this category as described above, poses high risk of exacerbating the extant over-medicalization and over-diagnosis of this disorder category.
• A recent publication by the Task Force, The Conceptual Evolution of DSM-5 (Regier, Narrow, Kuhl, & Kupfer, 2011), states that the primary goal of DSM-5 is “to produce diagnostic criteria and disorder categories that keep pace with advances in neuroscience.” We believe that the primary goal of DSM-5 should be to keep pace with advances in all types of empirical knowledge (e.g., psychological, social, cultural, etc.).
Taken together, these proposed changes seem to depart from DSM’s 30-year “atheoretical” stance in favor of a pathophysiological model. This move appears to overlook growing disenchantment with strict neurobiological theories of mental disorder (e.g., “chemical imbalance” theories such as the dopamine theory of schizophrenia and the serotonin theory of depression), as well as the general failure of the neo-Kraepelinian model for validating psychiatric illness. Or in the words of the Task Force:
“…epidemiological, neurobiological, cross-cultural, and basic behavioral research conducted since DSM-IV has suggested that demonstrating construct validity for many of these strict diagnostic categories (as envisioned most notably by Robins and Guze) will remain an elusive goal” (Kendler, Kupfer, Narrow, Phillips, & Fawcett, 2009, p. 1).
We thus believe that a move towards biological theory directly contradicts evidence that psychopathology, unlike medical pathology, cannot be reduced to pathognomonic physiological signs or even multiple biomarkers. Further, growing evidence suggests that though psychotropic medications do not necessarily correct putative chemical imbalances, they do pose substantial iatrogenic hazards. For example, the increasingly popular neuroleptic (antipsychotic) medications, though helpful for many people in the short term, pose the long-term risks of obesity, diabetes, movement disorders, cognitive decline, worsening of psychotic symptoms, reduction in brain volume, and shortened lifespan (Ho, Andreasen, Ziebell, Pierson, & Magnotta, 2011; Whitaker, 2002, 2010). Indeed, though neurobiology may not fully explain the etiology of DSM-defined disorders, mounting longitudinal evidence suggests that the brain is dramatically altered over the course of psychiatric treatment.
Conclusions
In sum, we have serious reservations about the proposed content of the future DSM-5, as we believe that the new proposals pose the risk of exacerbating longstanding problems with the current system. Many of our reservations, including some of the problems described above, have already been articulated in the formal response to DSM-5 issued by the British Psychological Society (BPS, 2011) and in the email communication of the American Counseling Association (ACA) to Allen Frances (Frances, 2011b).
In light of the above-listed reservations concerning DSM-5’s proposed changes, we hereby voice agreement with BPS that:
• “…clients and the general public are negatively affected by the continued and continuous medicalization of their natural and normal responses to their experiences; responses which undoubtedly have distressing consequences which demand helping responses, but which do not reflect illnesses so much as normal individual variation.”
• “The putative diagnoses presented in DSM-V are clearly based largely on social norms, with ‘symptoms’ that all rely on subjective judgments, with little confirmatory physical ‘signs’ or evidence of biological causation. The criteria are not value-free, but rather reflect current normative social expectations.”
• “… [taxonomic] systems such as this are based on identifying problems as located within individuals. This misses the relational context of problems and the undeniable social causation of many such problems.”
• There is a need for “a revision of the way mental distress is thought about, starting with recognition of the overwhelming evidence that it is on a spectrum with ‘normal’ experience” and the fact that strongly evidenced causal factors include “psychosocial factors such as poverty, unemployment and trauma.”
• An ideal empirical system for classification would not be based on past theory but rather would “ begin from the bottom up – starting with specific experiences, problems or ‘symptoms’ or ‘complaints’.”
The present DSM-5 development period may provide a unique opportunity to address these dilemmas, especially given the Task Force’s willingness to reconceptualize the general architecture of psychiatric taxonomy. However, we believe that the proposals presented on www.dsm5.org are more likely to exacerbate rather than mitigate these longstanding problems. We share BPS’s hopes for a more inductive, descriptive approach in the future, and we join BPS in offering participation and guidance in the revision process.
References
American Psychiatric Association (2011). DSM-5 Development. Retrieved from http://www.dsm5.org/Pages/Default.aspx
British Psychological Society. (2011) Response to the American Psychiatric Association: DSM-5 development.
Retrieved from http://apps.bps.org.uk/_publicationfiles/consultation-responses/DSM-5%202011%20-%20BPS%20response.pdf
Compton, M. T. (2008). Advances in the early detection and prevention of schizophrenia.
Medscape Psychiatry & Mental Health. Retrieved from http://www.medscape.org/viewarticle/575910
Frances, A. (2010). The first draft of DSM-V. BMJ. Retrieved from http://www.bmj.com/content/340/bmj.c1168.full
Frances, A. (2011a). DSM-5 approves new fad diagnosis for child psychiatry: Antipsychotic use
likely to rise. Psychiatric Times. Retrieved from http://www.psychiatrictimes.com/display/article/10168/1912195
Frances, A. (2011b). Who needs DSM-5? A strong warning comes from professional counselors
[Web log message]. Psychology Today. Retrieved from http://www.psychologytoday.com/blog/dsm5-in-distress/201106/who-needs-dsm-5
Hanssen, M., Bak, M., Bijl, R., Vollebergh, W., & van Os, J. (2005). The incidence and outcome of subclinical psychotic experiences in the general population. British Journal of Clinical Psychology, 44, 181-191.
Ho, B-C., Andreasen, N. C., Ziebell, S., Pierson, R., & Magnotta, V. (2011). Long-term antipsychotic treatment and brain volumes. Archives of General Psychiatry, 68, 128-137.
Johns, L. C., & van Os, J. (2001). The continuity of psychotic experiences in the general population. Clinical Psychology Review, 21, 1125-1141.
Kendell, R., & Jablensky, A. (2003). Distinguishing between the validity and utility of psychiatric diagnoses. The American Journal of Psychiatry, 160, 4-11.
Kendler, K., Kupfer, D., Narrow, W., Phillips, K., & Fawcett, J. (2009, October 21). Guidelines
for making changes to DSM-V. Retrieved August 30, 2011, from
http://www.dsm5.org/ProgressReports/Documents/Guidelines-for-Making-Changes-to-DSM_1.pdf
Livesley, W. J. (2010). Confusion and incoherence in the classification of Personality Disorder: Commentary on the preliminary proposals for DSM-5. Psychological Injury and Law, 3, 304-313.
Moran, M. (2009). DSM-V developers weigh adding psychosis risk. Psychiatric News Online.
Retrieved from http://pn.psychiatryonline.org/content/44/16/5.1.full
Regier, D. A., Narrow, W. E., Kuhl, E. A., & Kupfer, D. J. (2011). The conceptual evolution of DSM-5. Arlington, VA: American Psychiatric Publishing.
Schatzberg, A. F., Scully, J. H., Kupfer, D. J., & Regier, D. A. (2009). Setting the record straight: A response to Frances commentary on DSM-V. Psychiatric Times, 26. Retrieved from http://www.psychiatrictimes.com/dsm/content/article/10168/1425806
Whitaker, R. (2002). Mad in America. Cambridge, MA: Basic Books. Also see http://www.madinamerica.com/madinamerica.com/Schizophrenia.html
Whitaker, R. (2010). Anatomy of an epidemic. New York, NY: Random House.