Questions raised on ICD-11 Beta draft re: Bodily distress disorder
July 24, 2014
Post #311 Shortlink: http://wp.me/pKrrB-3Yh
Screenshot: ICD-11 Beta drafting platform, public version, July 31, 2014; Chapter 06 Mental and behavioural disorders: Bodily distress disorder.
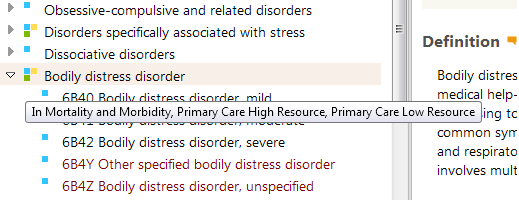
Joint Linerarization for Mortality and Morbidity Statistics view selected; “show availability in main linearizations” view selected. Categories designated with three coloured key hover text: “In Mortality and Morbidity, Primary Care High Resource, Primary Care Low Resource. Categories designated with single blue key hover text: “In Mortality and Morbidity.”
Yesterday, I left the following comments and questions for TAG Mental Health Managing Editors via the ICD-11 Beta drafting platform.
In order to read the comment in situ you will need to be registered with the Beta drafting platform, logged in, then click on the grey and orange quote icon at the end of the category Title.
http://apps.who.int/classifications/icd11/browse/f/en#/http://id.who.int/icd/entity/1121638993
Bodily distress disorder, severe
Comments on title
Suzy Chapman 2014-Jul-23 – 14:01 UTC
Definitions for three uniquely coded severities for Bodily distress disorder: Mild; Moderate; Severe, have recently been inserted into the Beta draft.
The Definition for Bodily distress disorder (BDD) and its three severity characterizations appears to be based on the BDD disorder descriptions in the 2012 Creed, Gureje paper: Emerging themes in the revision of the classification of somatoform disorders [1].
As conceptualized by the ICD-11 Expert Working Group on Somatic Distress and Dissociative Disorders (S3DWG), BDD is proposed to replace the seven ICD-10 Somatoform disorders categories F45.0 to F45.9, and F48.0 Neurasthenia.
The S3DWG’s BDD eliminates the requirement that symptoms be “medically unexplained” as the central defining feature; focuses on identification of positive psychobehavioural responses (excessive preoccupation with bodily symptoms, unreasonable illness fear, frequent or persistent healthcare utilization, activity avoidance for fear of damaging the body) in response to any (unspecific) persistent, distressing, single or multiple bodily symptom(s), resulting in significant impairment of functioning or frequent seeking of reassurance; makes no assumptions about aetiology, and in “[d]oing away with the unreliable assumption of its causality, the diagnosis of BDD does not exclude the presence of (…) a co-occurring physical health condition.”
The S3DWG’s BDD has no requirement for symptom counts, or for symptom patterns or symptom clusters from body or organ systems, which describes a disorder framework with good concordance with DSM-5 Somatic Symptom Disorder (SSD).
According to the Beta draft, BDD’s three severity specifiers are proposed to be characterized on the basis of the extent to which responses to persistent, distressing bodily symptoms are perceived as excessive and on the degree of impairment, not on the basis of number of bodily symptoms and number of body or organ systems affected.
In comparison, psychobehavioural responses do not form part of Fink et al’s (2010) Bodily Distress Syndrome criteria. BDS’s criteria and two severities are based on symptom patterns from body systems (a BDS Modest, single-organ type and a BDS Severe, Multi-organ type).
In 2012, the Lam et al paper [2], set out emerging proposals for the ICD-11 Primary Care Consultation Group’s (PCCG) recommendations for a “Bodily stress syndrome (BSS).”
The PCCG’s proposals described a disorder construct that had good concordance with Fink et al’s Bodily Distress Syndrome, drawing heavily on Fink et al’s criteria set. Although at that point, the PCCG proposed to incorporate some SSD-like psychobehavioural features within their tentative criteria. The PCCG appeared to be proposing a modified version of the Fink et al (2010) BDS construct.
In an Ivbijaro G, Goldberg D (June 2013) editorial [3], the co-authors advance the position that the forthcoming revision of ICD provides an opportunity to include BDS in a revised classification for primary care. According to this June 2013 editorial, the PCCG’s proposal for a modified BDS disorder construct, which it had earlier proposed to call “Bodily stress syndrome (BSS),” appears to have been revised to using the Fink et al “Bodily distress syndrome (BDS)” term.
The editorial implies that BDS (which subsumes the so-called “functional somatic syndromes,” CFS, ME, IBS, Fibromyalgia, chronic pain disorder, MCS and some others, under a single, overarching disorder) was expected to be progressing, imminently, to ICD-11 field trials.
(A revision of the earlier BSS disorder name is not discussed within the editorial; nor whether any modifications to, or deviance from a “pure” BDS construct and criteria were being recommended for the purposes of field testing; nor are the alternative proposals of the S3DWG referenced or discussed; nor are the views of the Revision Steering Group on either set of proposals discussed.)
According to Lam et al (2012) and Ivbijaro and Goldberg (June 2013), the model proposed is that of “autonomic over-arousal,” which the authors consider may be responsible for most or all of the somatic symptoms that are experienced.
Again, compare with the S3DWG’s BDD construct, which makes no assumptions about aetiology and does not exclude the presence of a co-occurring physical health condition, whereas, for both Lam et al’s 2012 BSS and for Fink et al’s BDS, “If the symptoms are better explained by another disease, they cannot be labelled BDS.”
Potential for confusion between divergent disorder constructs:
The term “Bodily distress disorder” and the term “Bodily distress syndrome” (Fink et al, 2010), which is already operationalized in Denmark in research and clinical settings, are often seen being used interchangeably in the literature. For example, in this very recent editorial by Rief and Isaac [4]. Also in papers by Fink and others from 2007 onwards [5].
However, the S3DWG’s defining of a “Bodily distress disorder” construct has stronger conceptual alignment and criteria congruency with DSM-5’s SSD and poor conceptual and criteria congruency with Fink et al’s BDS. That SSD and BDS are very different concepts is acknowledged by Fink, Creed and Henningsen [6] [7].
Although the 2013 Ivbijaro and Goldberg editorial implies that Fink et al’s BDS construct was going forward to ICD-11 field testing, it is the S3DWG’s Bodily distress disorder name and construct that has been entered into the Beta draft – the construct that has stronger conceptual alignment with DSM-5’s SSD.
So the current proposals and intentions for field testing a potential replacement for the SDs remain unclear. This is severely hampering professional and consumer stakeholder scrutiny, discourse and input.
Four questions for TAG Mental Health Managing Editors:
1. Have the S3DWG sub working group, the PCCG working group and the Revision Steering Group reached consensus over a potential replacement framework and disorder construct for ICD-10’s Somatoform disorders and F48.0 Neurasthenia, and the ICD-10-PHC categories: F45 Unexplained somatic symptoms/medically unexplained symptoms, and F48 Neurasthenia?
2. Which recommendations are being progressed to international field testing and does ICD-11 intend to release the protocol or other information on finalized characteristics, diagnostic guidelines, criteria, inclusions, exclusions, differential diagnoses etc, that are planned to be used for the field tests and which would provide the level of detail lacking in the public version of the Beta drafting platform?
3. If, in the context of ICD-11 usage, the S3DWG working group’s proposal for a replacement for the Somatoform disorders remains for a disorder model with good concordance with the DSM-5 SSD construct, what is the rationale for proposing to name this disorder “Bodily distress disorder”?
4. Have the S3DWG, PCCG and Revision Steering Group given consideration to the significant potential for confusion if its replacement construct for the Somatoform disorders has greater conceptual alignment with the SSD construct but is assigned a disorder name that sounds very similar to, and is already being used interchangeably with an operationalized but divergent construct and criteria set?
References:
1. Creed F, Gureje O. Emerging themes in the revision of the classification of somatoform disorders. Int Rev Psychiatry. 2012 Dec;24(6):556-67. http://www.ncbi.nlm.nih.gov/pubmed/23244611 [Full text behind paywall]
2. Lam TP, Goldberg DP, Dowell AC, Fortes S, Mbatia JK, Minhas FA, Klinkman MS: Proposed new diagnoses of anxious depression and bodily stress syndrome in ICD-11-PHC: an international focus group study. Family Practice (2013) 30 (1): 76-87. Full free text: http://fampra.oxfordjournals.org/content/30/1/76.long
3. Ivbijaro G, Goldberg D. Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (MUS). Ment Health Fam Med. 2013 Jun;10(2):63-4. Full free text available on 2014/6/1: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3822636/pdf/MHFM-10-063.pdf
4. Rief W, Isaac M. The future of somatoform disorders: somatic symptom disorder, bodily distress disorder or functional syndromes? Curr Opin Psychiatry (2014). Full free: http://journals.lww.com/co-psychiatry/Fulltext/2014/09000/The_future_of_somatoform_disorders___somatic.2.aspx
5. Fink P, Toft T, Hansen MS, Ornbol E, Olesen F. Symptoms and syndromes of bodily distress: an exploratory study of 978 internal medical, neurological, and primary care patients. Psychosom Med. 2007 Jan;69(1):30-9.
6. Medically Unexplained Symptoms, Somatisation and Bodily Distress: Developing Better Clinical Services, Francis Creed, Peter Henningsen, Per Fink (Eds), Cambridge University Press, 2011.
7. Discussions between Prof Francis Creed and Prof Per Fink during Research Clinic for Functional Disorders Symposium presentations, Aarhus University Hospital, May 15, 2014, noted that Fink et al BDS and DSM-5 SSD are “very different concepts.”
September symposium presentation on BDD:
In September, Professor Oye Gureje (who chairs the ICD-11 Expert Working Group on Somatic Distress and Dissociative Disorders), will be presenting on Proposals and evidence for the ICD-11 classification of Bodily Distress Disorders, as part of series of symposia on the development of the ICD-11 chapter for mental and behavioural disorders, at the World Psychiatric Association XVI World Congress in Madrid, Spain, 14–18 September 2014.
Unfortunately, I cannot attend this September symposia but would be pleased to hear from anyone who may be planning to attend.
Caveats: The ICD-11 Beta drafting platform is not a static document: it is a work in progress, subject to daily edits and revisions, to field test evaluation and to approval by ICD Revision Steering Group and WHO classification experts. Not all new proposals may survive ICD-11 field testing. Chapter numbering, codes and Sorting codes currently assigned to ICD categories may change as chapters and parent/child hierarchies are reorganized. The public version of the Beta draft is incomplete; not all “Content Model” parameters display or are populated; the draft may contain errors and category omissions.
Further reading:
Dx Revision Watch Post: Definitions for three severities of “Bodily distress disorder” now inserted in ICD-11 Beta draft, July 19, 2014 http://wp.me/pKrrB-3X9
Dx Revision Watch Post: Editorial: Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (Goldberg and ICD-11-PHC), June 3, 2014: http://wp.me/pKrrB-3Uh








