DSM-5 rejects call for urgent reconsideration of new “Somatic Symptom Disorder” category
January 17, 2013
DSM-5 rejects call from lead psychiatrist for DSM-IV Task Force for urgent reconsideration of new “Somatic Symptom Disorder” category
Post #219 Shortlink: http://wp.me/pKrrB-2C0
Today, Allen Frances, M.D., publishes a follow-up to our December 8 commentary in which we set out the implications for all chronic illness patient populations of misdiagnosis with “Somatic Symptom Disorder (SSD)” or misapplication of an additional diagnosis of “SSD.”
In the second of three commentaries, Dr Frances reports on the outcome of his representations to the DSM-5 Somatic Symptom Disorder Work Group, key APA Board of Trustees office holders and DSM-5’s Task Force chair and vice-chair, for urgent reconsideration of this new “catch-all” mental health disorder.
The texts for DSM-5 are expected to be finalized for the publishers by the end of this month.
Dr Frances’ first commentary on SSD is approaching 20,000 views and has received over 300 comments on Psychology Today, alone. It is also published at Huffington Post and at Education Update and widely circulated on other platforms.
There has been an overwhelming response to our concerns with comments pouring in from patients with diverse chronic illnesses and medical conditions including Ehlers-Danlos Syndrome, Interstitial Cystitis, Behcet’s disease, Endometriosis, Lupus, Hashimotos thyroid disorder, Hughes Syndrome, Pancreatitis and Chronic Lyme disease –patients whose symptoms had been dismissed for years before finally receiving a diagnosis or who are still struggling to obtain a diagnosis, many of whom had been mislabelled with a somatoform disorder.
We’ve also received many emails from patients and international patient organizations.
Please circulate this follow-up commentary. I am particularly keen to reach platforms for patients with common chronic diseases and conditions – cancer, heart disease, diabetes, COPD, MS, RA, chronic pain; also Lyme disease, chemical injury and rare diseases, IBS and Fibromyalgia, ME and CFS.
Allen Frances, M.D., was chair of the DSM-IV Task Force and of the department of psychiatry at Duke University School of Medicine, Durham, NC. He is currently professor emeritus at Duke.
Psychology Today
DSM5 in Distress
The DSM’s impact on mental health practice and research
by Allen Frances, M.D.Published on January 16, 2013 by Allen J. Frances, M.D., in DSM5 in Distress
Bad News: DSM 5 Refuses To Correct Somatic Symptom Disorder
Medical Illness Will Be Mislabeled Mental Disorder“Many of you will have read a previous blog prepared by Suzy Chapman and me that contained alarming information about the new DSM 5 diagnosis ‘Somatic Symptom Disorder.’
“SSD is defined so over inclusively by DSM 5 that it will mislabel 1 in 6 people with cancer and heart disease; 1 in 4 with irritable bowel and fibromyalgia; and 1 in 14 who are not even medically ill.
“I hoped to be able to influence the DSM 5 work group to correct this in 2 ways: 1) by suggesting improvements in the wording of the SSD criteria set that would reduce mislabeling; and 2) by letting them know how much opposition they would face from concerned professionals and an outraged public if DSM 5 failed to slam on the brakes while there was still time…”
Read on here:
Bad News: DSM 5 Refuses To Correct Somatic Symptom Disorder
Medical Illness Will Be Mislabeled Mental Disorder
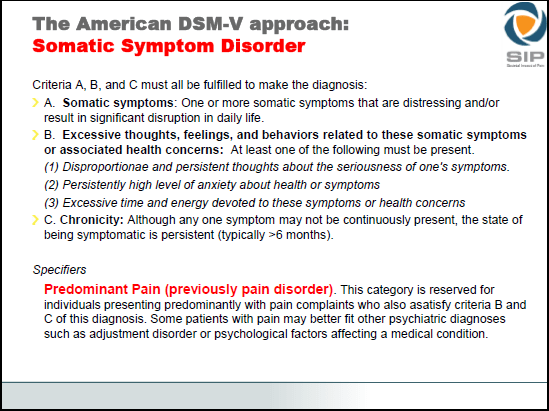
The most recent proposals for new category “J 00 Somatic Symptom Disorder”
IASP and the Classification of Pain in ICD-11 Prof. Dr. Winfried Rief, University of Marburg, Germany
Slide 9
Ed: Note that the requirement for “at least two from the B type criteria” was reduced to “at least one from the B type criteria” for the third iteration of draft proposals. This lowering of the threshold is presumably in order to accommodate the merging of the previously proposed “Simple Somatic Symptom Disorder” category into the “Complex Somatic Symptom Disorder” category, a conflation now proposed to be renamed to “Somatic Symptom Disorder,” also the disorder section name. A revised “Rationale/Validity” PDF document was not issued for the third and final draft. A brief, revised “Rationale” text was published on a Tab Page for the Somatic Symptom Disorder proposal and criteria but is no longer accessible.
Proposals, criteria and rationales, as posted for the third draft in May 2012, were removed from the DSM-5 Development website on November 15, 2012 and placed behind a non public log in. Criteria as they had stood for the third draft can no longer be viewed but are set out on Slide 9 in this presentation, which note, does not include three, optional Severity Specifiers that were included with the third draft criteria.
Related material
Mislabeling Medical Illness As Mental Disorder: The Eleventh DSM-5 Mistake, Psychology Today, DSM5 in Distress, Allen Frances, MD, December 8, 2012
Somatic Symptom Disorder could capture millions more under mental health diagnosis, Suzy Chapman
Submission to Somatic Symptom Disorder Work Group in response to third draft proposals, Suzy Chapman
Additional commentary
Oak Park Behavioral Medicine, Mind Your Body blog
Dr Tiffany Taft, Ph.D., Northwestern University, December 13, 2012
IBS Impact IBS Impact blog
Proposed DSM-5 Criteria May Unfairly Label Physical Conditions as Psychological Disorders