June 3, 2014
by admindxrw
An editorial and four papers on the theme of medically unexplained symptoms, first published in the June 2013 issue of Mental Health in Family Medicine and embargoed until June 1, 2014, are now accessible for free at: http://www.ncbi.nlm.nih.gov/pmc/issues/229531/
Mental Health in Family Medicine is the official journal of The World Organization of Family Doctors (Wonca) Working Party on Mental Health.
The editorial: Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (MUS), is co-authored by Prof Gabriel Ivbijaro and Prof Sir David Goldberg.
Prof Ivbijaro is Editor in Chief, Mental Health in Family Medicine, a past chair of Wonca Working Party on Mental Health and was elected president elect of the World Federation of Mental Health in August 2013.
Prof Goldberg chairs the WHO Primary Care Consultation Group (PCCG) that is leading the development of the primary care classification of mental and behavioural disorders for ICD-11 (known as ICD-11-PHC).
This report sets the editorial into context.
++
ICD-11 PHC
ICD-10 PHC (sometimes written as ICD-10-PHC or ICD10-PHC or ICD-10 PC), is a simplified version of the WHO’s ICD-10 chapter for mental and behavioural disorders for use in general practice and primary health care settings. This system has rough but not exact equivalence to selected of the mental disorders in the core ICD-10 classification.
The ICD-10 PHC describes 25 disorders commonly managed within primary care as opposed to circa 450 classified within Chapter V of ICD-10.
A revised edition, ICD-11 PHC, is being developed for use by clinicians and (often non-specialist) health-care workers in a wide range of global primary care settings and low- and middle-income countries.
The primary care version of the ICD-11 mental and behavioural disorders chapter is being developed simultaneously with the specialty settings version. Disorders that survive the ICD-11 PHC field tests require a corresponding disorder in the main ICD-11 classification.
The PCCG work group is developing and field testing 28 mental disorders for ICD-11 PHC, which includes making recommendations to the International Advisory Group for a potential replacement for the existing ICD-10 PHC category, F45 Unexplained somatic symptoms/medically unexplained symptoms.
A second ICD-11 working group, the Expert Working Group on Somatic Distress and Dissociative Disorders (S3DWG), is advising on the revision of ICD-10’s Somatoform disorders in parallel with the PCCG and has proposed an alternative disorder construct.
Thus far, neither working group has commented publicly on the alternative proposals presented by the other group, how the two groups interrelate, whether they are expected to reach consensus over a potential new conceptual framework to replace the existing Somatoform disorders, or to what extent consensus has been reached.
No public progress reports are being published by either group, or by the International Advisory Group, and those monitoring and reporting on the revision of these ICD-10 Chapter V categories rely on journal papers, editorials, symposia presentations, internal ICD Revision summary reports and meeting materials and on the limited content in the public version of the ICD-11 Beta drafting platform to piece together updates.
++
Does this editorial advance our understanding of current proposals?
Key point: this Ivbijaro and Goldberg editorial is now over 12 months old and should be read with the caveat that proposals by the PCCG working group may have been revised since the editorial was first published.
As a source of information on the current status of proposals by the Primary Care Consultation Group (PCCG), this editorial is problematic.
Firstly, it is over 12 months old and the PCCG’s proposals may have undergone further revision since the editorial was submitted for publication.
At the time of submission, the authors anticipated imminent field testing for ICD-11 PHC but the projected start dates for internet and clinic-based field testing, which will assess utility of proposed ICD-11 diagnostic guidelines in different types of primary care settings with particular focus on low- and middle-income countries, may be delayed. (It is on record that field tests were running behind schedule and there have been funding shortfalls, two factors in WHO’s decision, earlier this year, to shift WHA approval of ICD-11 from 2015 to 2017 to allow more time for incorporation of field test results.*)
Secondly, the editorial does not declare Prof Goldberg’s interest as chair of the PCCG. It does not clarify whether the views and opinions expressed within the editorial represent the views and opinions of its authors or represent the official positions of the PCCG working group, or of the International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders, or of the ICD-11 Revision Steering Group.
Thirdly, its brevity. This is a short editorial – not a paper:
• it does not discuss the PCCG’s rationales for the changes made to its own proposals, as published in 2012.
• it does not retrospectively review and compare the PCCG’s 2012 proposals for a construct which the group proposed to call, at that point, Bodily stress syndrome, with the 2012 proposals of the Expert Working Group on Somatic Distress and Dissociative Disorders (S3DWG) for an alternative construct called Bodily distress disorder.
• it does not compare the PCCG’s revised proposals, as they stood in June 2013, with the S3DWG’s proposals, at that point.
• crucially, it does not clarify why, if the PCCG’s June 2013 proposals were expected to be progressed to field trials, it is the S3DWG’s Bodily distress disorder diagnostic construct that has been listed and defined in the Beta draft for the Foundation, Mortality and Morbidity, Primary Care High Resource, Primary Care Low Resource linearizations.
Key points: It is difficult to disentangle the authors’ views and opinions from official position of the PCCG working group or the International Advisory Group. The editorial provides no discussion of the S3DWG’s alternative proposals or whether any consensus between the two groups had been reached. The opinions of the International Advisory Group on both sets of proposals are not discussed.
++
What new information does this June 2013 editorial provide since the 2012 Lam et al paper?
• that the authors consider the Fink P, Schröder A. 2010 paper [1] provides evidence that the term Bodily Distress Syndrome has both face and content validity.
• that the authors consider the concept Bodily Distress Syndrome as “a possible diagnosis that captures the range of presentations in primary care, which may be acceptable to both patient and medical professional”, for which the authors list “a range of poorly defined disorders [that include] chronic fatigue syndrome (CFS), fibromyalgia, irritable bowel syndrome (IBS), chronic pain syndrome, hyperventilation syndrome, non-cardiac chest pain and somatoform disorder.”
• that the authors consider the forthcoming revision of the ICD provides an opportunity to include BDS in a revised classification for primary care, the ICD11-PHC, which is planned to be field tested in eight countries.
• that “not only has BDS replaced ‘medically unexplained symptoms’, but also ‘health anxiety’ has replaced ‘hypochondriasis'” and that the field trials “would examine whether primary care physicians wish to distinguish health anxiety (which may have few or indeed no somatic symptoms) from BDS (which by definition has at least three different somatic symptoms).”
According to the editorial, the PCCG had evidently revised its proposal for what to call its new disorder category since publication of the Lam et al paper, in 2012.
In 2012, the PCCG’s proposed term for ICD-11 PHC was Bodily stress syndrome (BSS). In this June 2013 editorial, the authors are using the term, Bodily distress syndrome (BDS).
In 2012, criteria for the PCCG’s BSS had included the requirement for psychobehavioural responses, which do not form part of the Fink et al 2010 BDS criteria – which are based on symptom patterns.
The editorial does not clarify whether, in June 2013, the PCCG (or its chair) was now advancing that the BDS construct and criteria should progress unmodified for ICD-11 PHC testing and evaluation, that is, in the form already operationalized in research and clinical settings in Denmark or would be modified for the purpose of ICD-11 PHC field trials, or to what extent.
(There is no revised criteria set included in this editorial for comparison with the detailed disorder descriptions and criteria set that had been included in Appendix 2 of the 2012 Lam et al paper.)
Key point: The editorial provides no details or discussion of a 2013 field trial protocol. The most recent disorder descriptions, diagnostic guidelines and criteria proposed by the PCCG are not in the public domain. It is not known whether a field trial protocol has been finalized, whether or when it will be made available for public scrutiny, or whether field trials have started yet.
++
Before reading the editorial please read the appended notes and if you are linking to the editorial on social media or forums, please also include a link back to this report because it is important that this editorial is placed into context.
+++
Ment Health Fam Med.
2013 Jun;10(2):63-4.
Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (MUS).
Ivbijaro G, 1 Goldberg D. 2
Author information
1 Editor-in-Chief Mental Health in Family Medicine, Medical Director, Waltham Forest Community and Family Health Services, and Vice President (Europe), World Federation for Mental Health.
2 Professor Emeritus and Fellow, King’s College, London.PMID: 24427171
[PubMed] PMCID: PMC3822636 [Available on 2014/6/1]
+++
Two ICD Revision working groups – two sets of proposals published in 2012:
In their respective 2012 journal papers, the two working groups presented divergent conceptual proposals and neither group refers to the work being undertaken by the other group.
The 17 member Expert Working Group on Somatic Distress and Dissociative Disorders (the S3DWG) is an ICD Revision sub working group advising specifically on the revision of ICD-10’s Somatoform disorders.
Prof emeritus Francis Creed (a former DSM-5 Somatic Symptom Disorder work group member) is a member of the S3DWG, and the group is chaired by Prof Oye Gureje.
In late 2012, Creed and Gureje published a paper which had included the S3DWG’s emerging proposals for a new, single diagnostic category that would subsume the existing Somatoform disorders categories F45.0 – F45.9 and Neurasthenia [2].
The S3DWG paper sets out the group’s remit which includes:
“To provide drafts of the content (e.g. definitions, descriptions, diagnostic guidelines) for somatic distress and dissociative disorder categories in line with the overall ICD revision requirements.
“To propose entities and descriptions that are needed for classification of somatic distress and dissociative disorders in different types of primary care settings, particularly in low- and middle-income countries.”
Which suggests that the proposals the S3DWG group are advancing are also being considered for utility in primary care and low resource settings, in parallel with those recommended by the PCCG.
The S3DWG’s 2012 paper had described a disorder model which it proposed to call Bodily distress disorder (BDD).
Key point: Although the Creed, Gureje 2012 paper does not acknowledge the congruency, the BDD disorder descriptions and criteria are conceptually close to DSM-5’s new Somatic symptom disorder (SSD).
With its
“much simplified set of criteria”; no assumptions about causality; elimination of the requirement that symptoms be “medically unexplained” as the central defining feature; inclusion of the presence of a co-occurring physical health condition; focus on identification of positive psychobehavioural responses (excessive preoccupation with symptoms, unreasonable illness fear, frequent or persistent healthcare utilization, activity avoidance for fear of damaging the body) in response to any (unspecific) persistent, distressing, single or multiple bodily symptoms; and with no requirement for symptom counts or symptom patterns from body or organ systems;
the group’s BDD construct had good concordance with DSM-5’s Somatic symptom disorder (SSD) and poor concordance with Fink et al’s Bodily Distress Syndrome.
++
The PCCG’s Bodily stress syndrome (BSS):
In contrast, the PCCG’s 2012 paper [3] had described a disorder construct which it proposed to call Bodily stress syndrome (BSS), that drew heavily on Fink et al’s 2010 Bodily Distress Syndrome (BDS) disorder model [4].
BSS would replace ICD-10-PHC’s F45 Unexplained somatic symptoms/medically unexplained symptoms category. Primary care’s Neurasthenia category would also be eliminated for ICD-11-PHC.
Based (theoretically) on the “autonomic over-arousal” model, the PCCG’s BSS required symptom patterns from body systems to meet the diagnosis.
But, “If the symptoms are accounted for by a known physical disease this is not BSS.”
Which also mirrors Fink et al’s BDS – “if the symptoms are better explained by another disease, they cannot be labelled BDS. The diagnosis is therefore exclusively made on the basis of the symptoms, their complexity and duration” [4].
But the tentative BSS criteria, as presented by Lam et al, in 2012, also incorporated some DSM-5 SSD-like psychobehavioural responses, viz, “The patient’s concern over health expresses itself as excessive time and energy devoted to these symptoms.” (A straight lift from DSM-5’s SSD criteria.)
Psychological and behavioural responses do not form part of the Fink et al 2010 BDS criteria and their inclusion within BSS appeared to be a tokenistic nod towards accommodation of DSM-5’s SSD into any new conceptual framework for ICD-11. (The rationale for their insertion into an otherwise BDS-like construct is not discussed within the 2012 paper.)
Key point: In 2012, whilst highly derivative of BDS and the influence of PCCG group member, Marianne Rosendal, is clear, the proposed BSS model could not be described as a “pure” BDS model.
++
How viable is BDS for incorporation into ICD-11?
The vice-chair of the PCCG is Dr Michael Klinkman, a GP who represents WONCA (World Organization of Family Doctors). Dr Klinkman is current convenor of WONCA’s International Classification Committee (WICC) that is responsible for the development of ICPC-2.
Dr Marianne Rosendal (Department of Public Health, Aarhus University), who has published with Prof Per Fink, is the European representative on WONCA’s International Classification Committee and a member of the PCCG.
In addition to the revision of ICD-10 and ICD-10-PHC, the ICPC-2 (International Classification of Primary Care, Second edition), which classifies patient data and clinical activity in the domains of general/family practice and primary care, is also under revision.
Per Fink and colleagues have been lobbying for their Bodily Distress Syndrome construct to be integrated into forthcoming classification systems and adopted as a diagnosis by primary care practitioners.*
*Budtz-Lilly A: The Research Unit for General Practice, School of Public Health, Aarhus University, Denmark. Bodily Distress Syndrome: A new diagnosis for functional disorders in primary care, EACLPP 2012 Conference Abstract, p 17.
++

There are a number of reasons why the International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders and the ICD Revision Steering Group might have difficulty justifying approval of any new disorder construct that seeks to arrogate the so-called “functional somatic syndromes,” CFS, IBS and Fibromyalgia, and subsume them under a new, overarching disorder category that also subsumes Neurasthenia and the Somatoform disorders.
• limited independent evidence for construct validity, utility and safety of application of BDS in adults and children.
• no requirements within BDS criteria for positive psychobehavioural features – location within the ICD-11 mental and behavioural disorders chapter is therefore problematic.
• potential data loss, data disaggregation problems and code mapping issues resulting from loss of discretely coded terms currently located within various ICD chapters outside the mental and behavioural disorders chapter; loss of backward compatibility with ICD-10 codes and with ICD-10-CA, ICD-10-GM, ICD-10-AM and other country modifications. (Some countries may take many years to transition to ICD-11, or an adaptation of ICD-11.) Potential incompatibility problems mapping to SNOMED-CT.
• unacceptability to patients and medical professionals
• medico-political sensitivities
• BDS and SSD are divergent constructs; a hybrid between BDS and SSD-like characteristics is conceptually problematic and would present difficulties if the intention is to harmonize ICD-11 with DSM-5 for this section of the classification [5].
• the DSM-5 to ICD-9/ICD-10-CM cross-walk already maps DSM-5 Somatic symptom disorder to ICD-9 code 300.82 (ICD-10-CM F45.1).
It has been proposed that Somatic symptom disorder is added to the U.S.’s forthcoming clinical modification as an inclusion term to F45.1, in the Tabular List and Index.* If approved by NCHS, ICD-10-CM and ICD-11 would lack congruency if a BDS-like disorder model were incorporated into ICD-11 to replace the existing Somatoform disorders, rather than an SSD-like model.**
*September 18-19, 2013 and March 19-20, 2014 NCHS/CMS ICD-10-CM Coordination and Management Committee meetings.
**Note: since early 2009, I have strongly opposed the introduction of SSD into the DSM-5, ICD-11 and ICD-10-CM, and I am not arguing, here, in favour of an SSD-like model to replace the existing ICD-10 Somatoform disorders. There is no public domain documentary evidence that the two ICD working groups are currently considering any alternative models as potential replacements for the Somatoform disorders.
++
Has Professor Fink achieved his goal?
Disorders that survive the ICD-11 PHC field tests must have an equivalent disorder in the main ICD-11 classification.
With the criteria’s lack of positive psychobehavioural features presenting barriers for location within the ICD-11 mental and behavioural disorders chapter and with a hybrid between BDS and SSD-like features conceptually problematic, fitting BDS into ICD-11 isn’t the shoo in that Rosendal, Fink and colleagues had hoped for.
At the presentations on Functional Disorders held at the Danish parliament (March 19, 2014), Prof Fink had stated that he and his colleagues had tried to get WHO to incorporate a section for a special group of disorders where BDS could be placed that was located neither in psychiatry nor in general medicine, but had not been successful. [Creating a new ICD chapter or new parent class within an existing chapter for “interface” disorders may possibly have been proposed to ICD Revision.]*
But if a “pure” BDS (or a modification of BDS for ICD usage) is progressed to field testing over the next year or two, it should perhaps be considered whether ICD Revision has agreed to field test the PCCG’s proposal as a “straw man” construct to disprove its clinical utility, reliability and acceptability, with the intention of defaulting, after field trial evaluation, to a disorder construct that is conceptually closer to SSD, if the latter is already the preference of the International Advisory Group and the ICD Revision Steering Group.
*See: Constanze Hausteiner-Wiehle and Peter Henningsen. Irritable bowel syndrome: Relations with functional, mental, and somatoform disorders World J Gastroenterol 2014 May 28; 20(20): 6024-6030 Full free text
“An overarching category of general (medical-psychiatry) interface disorders could be a helpful conceptualization for the many phenomena that are neither only somatic nor only mental [32,56,79]. The ICD-11, awaited in 2015, offers a new chance to do that. The concept of a bodily distress syndrome (BDS) offers another scientifically coherent common basis for the classification of different dimensional graduations of IBS [80].
++
WHO on Twitter:
On Feb 12, 2014, @WHO Twitter admin stated: “Fibromyalgia, ME/CFS are not included as Mental & Behavioural Disorders in ICD-10, there is no proposal to do so for ICD-11”. This position was additionally confirmed by Mr Gregory Härtl, Head of Public Relations/Social Media, WHO.
++
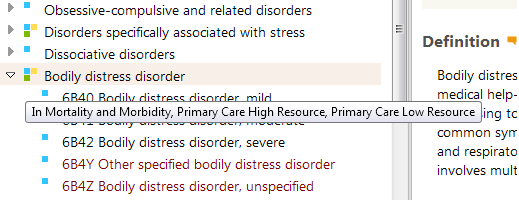
So what has been entered into the Beta drafting platform?
The term entered into the Beta platform (since February 2012) is Bodily distress disorder (the term favoured by the S3DWG working group) – not the term Bodily stress syndrome or Bodily Distress Syndrome.
A Definition for Bodily distress disorder was inserted around four months ago. There are no definitions or characterizations inserted yet for any of the three, uniquely coded severity specifiers (Mild; Moderate; Severe).
The psychological and behavioural features that characterize the disorder, as per the BDD Definition, are drawn from the disorder conceptualizations in the 2012 Creed, Gureje paper on emerging proposals for Bodily distress disorder which had described a disorder model with good concordance with DSM-5′s Somatic symptom disorder construct and poor concordance with Fink et al’s Bodily Distress Syndrome construct.
Key point: The term entered into the Beta drafting platform is Bodily distress disorder (the term favoured by the S3DWG working group) with a Definition based on disorder conceptualizations in the 2012 Creed, Gureje paper which had described a disorder model with good concordance with DSM-5′s Somatic symptom disorder and poor concordance with Fink et al’s Bodily Distress Syndrome construct.
++
This Dx Revision Watch post sets out (with screenshots) the most recent changes to the Beta drafting platform for the listing of BDD and the current Definition:
Recent changes to ICD-11 Beta drafting platform for “Bodily distress disorder”
++
Forthcoming symposium presentation:
In September, Oye Gureje (chair ICD-11 Expert Working Group on Somatic Distress and Dissociative Disorders), will be presenting on Proposals and evidence for the ICD-11 classification of Bodily Distress Disorders, as part of series of symposia on the development of the ICD-11 chapter on mental and behavioural disorders, at the World Psychiatric Association XVI World Congress, in Madrid, Spain, 14–18 September 2014 [6].
++
Field testing:
Field testing on a potential replacement for the ICD-10 Somatoform disorder categories is expected to be conducted over the next couple of years. Currently, there is no publicly available protocol or other information on the finalized characteristics, diagnostic guidelines, criteria, inclusions, exclusions, differential diagnoses etc. that are planned to be used for the field tests which would provide the level of detail lacking in the public version of the Beta drafting platform.
++
Requests for clarification repeatedly stonewalled:
ICD Revision has been asked several times, via the Beta drafting platform, to clarify its current proposals for the framework and disorder construct for a replacement for the ICD-10 Somatoform disorders. ICD Revision has also been asked to comment on the following:
“If, in the context of ICD-11 usage, the S3DWG working group’s proposal for a replacement for the Somatoform disorders remains for a disorder model with good concordance with DSM-5’s SSD construct, what is the rationale for proposing to name this disorder “Bodily distress disorder”?
“Have the S3DWG, PCCG and Revision Steering Group given consideration to the significant potential for confusion if its replacement construct for the Somatoform disorders has greater conceptual alignment with the SSD construct but is assigned a disorder name that sounds very similar to, and is already being used interchangeably with an operationalized but divergent construct and criteria set?”
No clarifications have been forthcoming to date. Lack of progress reports by both working groups and the degree of confusion over the content of the Beta draft is hampering stakeholder scrutiny, discourse and input. It’s not surprising few papers have been published to date reviewing and discussing ICD Revision’s proposals for a potential replacement for the ICD-10 Somatoform disorders when information on the most recent proposals for both working groups is proving so difficult to obtain.
It’s time medical and allied professionals and advocacy organizations demanded transparency from ICD Revision for its current intentions.
++
Caveats:
ICD-11 Beta is a work in progress, updated daily, not finalized. Proposals for new categories are subject to ongoing revision and refinement, to field test evaluation, may not survive field testing, and are not approved by ICD Revision or WHO.
++
References:
1. Fink P and Schröder A. One single diagnosis, bodily distress syndrome, succeeded to capture 10 diagnostic categories of functional somatic syndromes and somatoform disorders. Journal of Psychosomatic Research 2010;68:415–26.
2. Creed F, Gureje O. Emerging themes in the revision of the classification of somatoform disorders. Int Rev Psychiatry. 2012 Dec;24(6):556-67. [Abstract: PMID: 23244611]
3. Lam TP, Goldberg DP, Dowell AC, Fortes S, Mbatia JK, Minhas FA, Klinkman MS: Proposed new diagnoses of anxious depression and bodily stress syndrome in ICD-11-PHC: an international focus group study. Fam Pract Feb 2013 [Epub ahead of print July 2012]. [Abstract: PMID: 22843638] Full free text: http://fampra.oxfordjournals.org/content/30/1/76.long
4. http://funktionellelidelser.dk/en/about/bds/
5. Creed F, Fink P: Research Clinic for Functional Disorders Symposium presentations, Aarhus University Hospital, May 15, 2014.
That SSD and BDS are divergent constructs is also discussed in: Medically Unexplained Symptoms, Somatisation and Bodily Distress: Developing Better Clinical Services, Francis Creed, Peter Henningsen, Per Fink (Eds), Cambridge University Press, 2011.
6. World Psychiatric Association XVI World Congress, Madrid, Spain, 14–18 September 2014.