DSM-5 goes to press with ‘Somatic Symptom Disorder’ amid widespread professional and consumer concern
February 6, 2013
DSM-5 goes to press with ‘Somatic Symptom Disorder’ amid widespread professional and consumer concern
Post #224 Shortlink: http://wp.me/pKrrB-2EV
Update: On February 8, David J. Kupfer, MD, Chair, DSM-5 Task Force, published in defence of the ‘Somatic Symptom Disorder’ category on Huffington Post:
Last week, the American Psychiatric Association sent the next edition of its Diagnostic and Statistical Manual of Mental Disorders to the publishers.
When DSM-5 is released in May, it will introduce a new ‘catch-all’ diagnosis that could capture many thousands more patients under a mental disorder label.
Today, on Saving Normal at Psychology Today, Allen Frances, MD, who chaired the DSM-IV Task Force, publishes the third in a series of commentaries voicing considerable concern for all illness groups for the implications of an additional diagnosis of ‘Somatic Symptom Disorder.’
Why Did DSM 5 Botch Somatic Symptom Disorder?
Allen Frances writes:
“Once it is an official DSM 5 mental disorder, SSD is likely to be widely misapplied – to 1 in 6 people with cancer and heart disease and to 1 in 4 with irritable bowel syndrome and fibromyalgia…The definition of SSD is so loose it will capture 7% of healthy people (14 million in the US alone) suddenly making this pseudo diagnosis one of the most common of all ‘mental disorders’ in the general population.”
Suzy Chapman writes:
“These highly subjective, difficult to assess criteria have the potential for widespread misapplication, particularly in busy primary care settings – causing stigma to the medically ill and potentially resulting in poor medical workups, inappropriate treatment regimes and medico-legal claims against clinicians for missed diagnoses.
“Why has the Task Force and APA Board of Trustees been prepared to sign off on a definition and criteria set that lacks a body of rigorous evidence for its validity, safety and prevalence, thereby potentially putting the public at risk? And why is APA prepared to abrogate its duty of care as a professional body and expose its membership, physicians and the allied health professional end-users of its manual to the risk of potential law suits?”
From May, an additional mental health diagnosis of ‘Somatic Symptom Disorder’ (SSD) can be applied whether patients have diagnosed medical diseases like diabetes, angina, cancer or multiple sclerosis, chronic illnesses like IBS, fibromyalgia, chronic fatigue syndrome or chronic pain disorders, or unexplained conditions that have so far presented with bodily symptoms of unclear etiology.
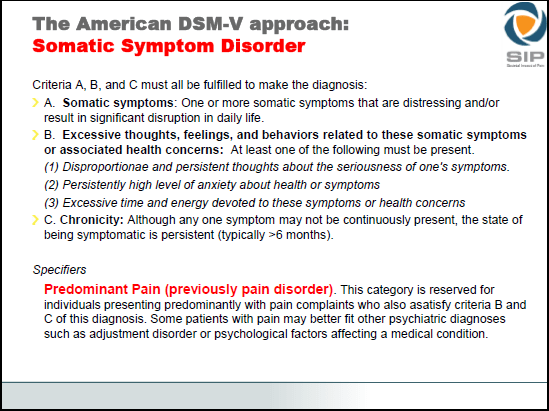
A person will meet the criteria for ‘Somatic Symptom Disorder’ by reporting just one or more bodily symptoms that are distressing or disruptive to daily life, that have persisted for at least six months, and having just one of the following three responses:
1) disproportionate, persistent thoughts about the seriousness of their symptoms;
2) persistently high level of anxiety about their health or symptoms;
3) devoting excessive time and energy to symptoms or health concerns.
In the DSM-5 field trials, 15% of the ‘diagnosed illness’ study group (the trials looked at patients with either cancer or coronary heart disease) met the criteria for an additional mental health diagnosis of SSD.
26% of patients who comprised the irritable bowel syndrome or fibromyalgia study group were coded for SSD.
A disturbingly high 7% of the ‘healthy’ control group were also caught by these overly-inclusive criteria.
Psychiatric creep
As the criteria stand, this new disorder will potentially result in a ‘bolt-on’ mental health diagnosis being applied to all chronic illnesses and medical conditions if the clinician decides the patient’s response to distressing symptoms is ‘excessive’ or their coping strategies are ‘maladaptive,’ or that they are ‘catastrophising’ or displaying ‘fear avoidance.’ Or if the practitioner feels the patient is spending too much time on the internet researching data, symptoms and treatments, or that their lives have become ‘dominated’ by ‘illness worries,’ they may be vulnerable to an additional diagnosis of SSD.
Patients with chronic, multiple bodily symptoms due to rare conditions or multi-system diseases like Behçet’s syndrome or Systemic lupus, which may take several years to diagnose, will also be vulnerable to misdiagnosis with a mental disorder.
There is no substantial body of research to support the validity, reliability or safety of the ‘Somatic Symptom Disorder’ diagnosis.
During the second public review of draft criteria for DSM-5, the ‘Somatic Symptom Disorder’ section received more submissions from advocacy organizations, patients, and professionals than almost any other disorder category. But rather than tighten up the criteria or subject the entire disorder section to independent scientific review, the SSD Work Group’s response has been to lower the threshold even further – potentially pulling even more patients under a mental disorder label.
The ‘Somatic Symptom Disorder’ Work Group has rejected eleventh hour calls from professionals and patients to review its criteria before going to print.
APA says there will be opportunities to reassess and revise DSM-5‘s new disorders, post publication, and that it intends to start work on a ‘DSM-5.1’ release. But patient groups, advocates and professionals are not reassured by a ‘publish first – patch later’ approach to science.
Read Parts One and Two, here:
Part One: Mislabeling Medical Illness As Mental Disorder | Allen Frances, December 8, 2012
Part Two: Bad News DSM-5 Refuses To Correct Somatic Symptom Disorder | Allen Frances, January 16, 2013
Notes for media, websites, bloggers:
1. The next edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) will be published by American Psychiatric Publishing Inc. in May 2013. It will be known as ‘DSM-5 ‘ and has been under development since 1999.
http://www.dsm5.org/Pages/Default.aspx
http://www.dsm5.org/Documents/DSM%205%20development%20factsheet%201-16-13.pdf
2. The American Psychiatric Association (APA) has spent $25 million on the development of DSM-5.
3. The Diagnostic and Statistical Manual of Mental Disorders is used by mental health and medical professionals for diagnosing and coding mental disorders. It is used by psychiatrists, psychologists, therapists, counselors, primary health care physicians, nurses, social workers, occupational and rehabilitation therapists and allied health professionals.
The DSM is also used for reimbursement and informs government, public health policy, courts and legal specialists, education, forensic science, prisons, drug regulation agencies, pharmaceutical companies and researchers. Diagnostic criteria defined within DSM determine what is considered a mental disorder and what is not, which treatments and therapies health insurers will authorise funding for, and for how long.
4. Four existing disorder categories in the DSM-IV ‘Somatoform Disorders’ section: somatization disorder [300.81], hypochondriasis [300.7], pain disorder, and undifferentiated somatoform disorder [300.82] will be eliminated and replaced with a single new category – ‘Somatic Symptom Disorder’ for DSM-5.
5. APA has held three stakeholder comment periods during which professional and public stakeholders have been invited to submit comment on the proposals for the revision of DSM-IV categories and criteria (in February-April 2010; May-June 2011; May-June 2012).
6. DSM-5 is slated for release at the American Psychiatric Association’s 166th Annual Meeting, San Francisco (May 18-22, 2013). The new manual is available for pre-order and will cost $199: http://www.psychiatry.org/dsm5
7. Allen Frances, MD, was chair of the DSM-IV Task Force and of the Department of Psychiatry at Duke University School of Medicine, Durham, NC; Dr Frances is currently professor emeritus, Duke.
8. Dr Frances blogs at DSM 5 in Distress, and Saving Normal at Psychology Today.
Mislabeling Medical Illness As Mental Disorder was published on December 8, 2012
Bad News DSM-5 Refuses To Correct Somatic Symptom Disorder was published on January 16, 2013
For additional information on ‘Somatic Symptom Disorder’:
Somatic Symptom Disorder could capture millions more under mental health diagnosis by Suzy Chapman for Dx Revision Watch, May 26, 2012
Suzy Chapman