CMS posts ICD-10-CM Release for 2015; confirms Partial Code Freeze extension; reminder, SSD proposals
May 24, 2014
Post #306 Shortlink: http://wp.me/pKrrB-3SJ
This report updates on the revised implementation date for ICD-10-CM, the revised Partial Code Freeze timeline, the ICD-10-CM Release for 2015 files, and a reminder of the deadline for objections to the insertion of DSM-5’s Somatic symptom disorder into ICD-10-CM.
[For reminder of deadline for objections to proposed insertion of Somatic symptom disorder into ICD-10-CM, skip to red subheading.]
On April 1, 2014, Bill H.R. 4302, known as the PAM Act (Protecting Access to Medicare Act), was signed into law by President Obama.
As a result of a quietly inserted clause piggybacking on this Bill, implementation of ICD-10-CM was delayed by a further year. Centers for Medicare & Medicaid Services (CMS) has confirmed that the effective implementation date for ICD-10-CM is now October 1, 2015.
Until that time, the codes in ICD-10-CM (the U.S. specific adaptation of the WHO’s ICD-10) are not valid for any purpose or use.
Partial Code Freeze
CMS has announced that the partial code freeze on updates to the ICD-9-CM and ICD-10-CM diagnosis and procedure codes will continue until October 1, 2015.
Between October 1, 2011 and October 1, 2016 revisions to ICD-10-CM/PCS will be for new diseases/new technology procedures, and any minor revisions to correct reported errors in these classifications. Regular (at least annual) updates to ICD-10-CM/PCS will resume on October 1, 2016.
The Partial Code Freeze document has been updated to reflect the revised Timeline and can be accessed here in PDF format Partial Code Freeze for ICD-9-CM and ICD-10
or text, below:
Partial Code Freeze for ICD-9-CM and ICD-10
The ICD-10 Coordination and Maintenance Committee (formerly the ICD-9-CM Coordination and Maintenance Committee) implemented a partial freeze of the ICD-9-CM and ICD-10 (ICD-10-CM and ICD-10-PCS) codes prior to the implementation of ICD-10 which would end one year after the implementation of ICD-10. There was considerable support for this partial freeze. On April 1, 2014, the Protecting Access to Medicare Act of 2014 (PAMA) (Pub. L. No. 113-93) was enacted, which said that the Secretary may not adopt ICD-10 prior to October 1, 2015. Accordingly, the U.S. Department of Health and Human Services expects to release an interim final rule in the near future that will include a new compliance date that would require the use of ICD-10 beginning October 1, 2015. The rule will also require HIPAA covered entities to continue to use ICD-9-CM through September 30, 2015. When published, links will be provided to this interim final rule at http://www.cms.gov/Medicare/Coding/ICD10/Statute_Regulations.html
The partial freeze will be implemented as follows:
• The last regular, annual updates to both ICD-9-CM and ICD-10 code sets were made on October 1, 2011.
• On October 1, 2012, October 1, 2013, and October 1, 2014 there will be only limited code updates to both the ICD-9-CM and ICD-10 code sets to capture new technologies and diseases as required by section 503(a) of Pub. L. 108-173.
• On October 1, 2015, there will be only limited code updates to ICD-10 code sets to capture new technologies and diagnoses as required by section 503(a) of Pub. L. 108-173. There will be no updates to ICD-9-CM, as it will no longer be used for reporting.
• On October 1, 2016 (one year after implementation of ICD-10), regular updates to ICD-10 will begin.
The ICD-10 Coordination and Maintenance Committee will continue to meet twice a year during the partial freeze. At these meetings, the public will be asked to comment on whether or not requests for new diagnosis or procedure codes should be created based on the criteria of the need to capture a new technology or disease. Any code requests that do not meet the criteria will be evaluated for implementation within ICD-10 on and after October 1, 2016 once the partial freeze has ended.
CDC has not yet updated its webpages to reflect the ICD-10-CM implementation delay or the revised Partial Code Freeze timeline.
SSD and ICD-10-CM/PCS Coordination and Maintenance Committee proposals
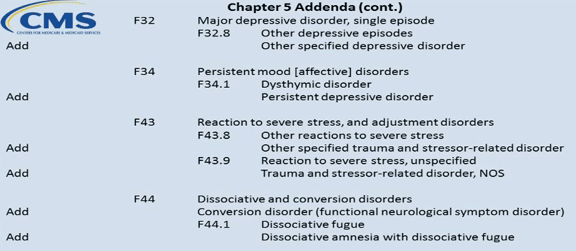
At the September 2013 and March 2014 Coordination and Maintenance Committee meetings, the American Psychiatric Association (APA) submitted numerous requests for addenda changes for new index entries and tabular inclusion terms for evaluation for implementation on October 1, 2015.
It is unclear whether requests for modifications submitted by APA and other requestors via these September and March meetings will be rolled forward for evaluation for implementation on and after the revised date of October 1, 2016 or whether these proposals will now need to be resubmitted at future C & M Committee meetings. (The next public meeting takes place September 23–24, 2014.)
I have approached NCHS for clarification.
If the proposals from these two meetings do require resubmitting, this would provide another opportunity to comment on the proposal to add the DSM-5’s new disorder term, Somatic symptom disorder, to the ICD-10-CM.
See earlier post: Update on proposal to add DSM-5′s Somatic symptom disorder to ICD-10-CM
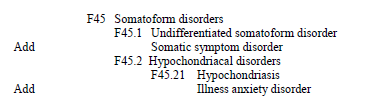
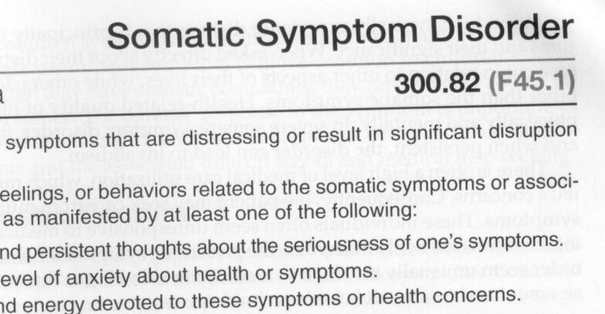
At the public Coordination and Maintenance Committee meeting on September 18–19, 2013, a proposal had been submitted to add Somatic symptom disorder (SSD) as an inclusion term to existing ICD-10-CM code F45.1 Undifferentiated somatoform disorder in the Tabular List Addendum (this also included addition to the Index).
Note: Proposal is not to create a unique code for SSD or to replace any of the existing ICD-10-CM somatoform disorders with SSD, but to add SSD as an inclusion term under an existing ICD-10-CM code, F45.1.
September 18–19, 2013 meeting Agenda, Page 45: PDF Agenda
The proposal to add somatic symptom disorder to the Index (under Disorder), was resubmitted at the public meeting on March 19–20, (reason unclear but a number of proposals for modifications to both the Tabular List and the Index from the September 2013 meeting were also duplicated at the March 2014 meeting).
March 19–20, 2014 meeting Agenda, Page 89: PDF Agenda
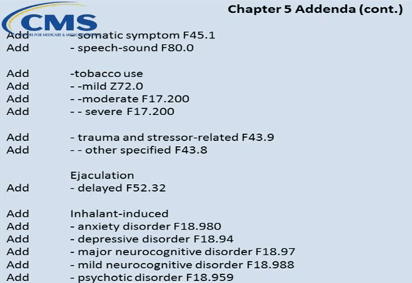
Any decisions made on the considerable number of proposals requested at last year’s September meeting are yet to be posted and possibly won’t be evident until the relevant Addendum is released.
In the DSM-5, Somatic symptom disorder is already cross-walked to ICD-9 code 300.82 (ICD-10-CM F45.1):
DSM-5 (Page 311)
Given that APA worked with CDC on the cross-walk between the new DSM-5 disorder terms and ICD-9/ICD-10-CM equivalent codes, NCHS’s Director will likely rubber stamp the APA’s proposals for insertion of SSD and a number of other new DSM-5 categories.
Nevertheless, I shall be putting in another objection before the June 20 deadline and I hope all stakeholders with concerns will strongly oppose the incorporation of this controversial new disorder construct into ICD-10-CM.
The deadline for comments on proposals requested at the March meeting is June 20th.
Send comments, by email, to NCHS to nchsicd9CM@cdc.gov
Not a small thing
Between 2010 and 2012, the SSD Work Group attracted considerable opposition across three stakeholder reviews to its radical proposals for a replacement for the somatoform disorders.
In late 2012 and early 2013, we saw a good deal of “outrage” in comments to articles by Allen Frances and myself here and here at Psychology Today and here in the BMJ, in response to the cavalier decision by the Task Force to barrel through with the SSD Work Group’s poorly validated disorder construct.
But I see little evidence of sustained opposition from U.S. professionals and patients over the September and March NCHS/CMS update and revision meeting proposals to insinuate SSD into ICD-10-CM.
At the moment, the proposal is for inserting SSD as an inclusion term under an existing category – not to create a unique code for SSD and not to replace the existing framework with SSD. At the September meeting, CDC’s Donna Pickett said:
“…And just to complete the package, there are other Tabular List proposals that appear on Page 45 and 46 that we would also invite your comments on. And again, with some of the terminology changes that Dr Regier has described the intent here is to make sure that if those terms are being used, that they do have a home somewhere within ICD-10-CM to facilitate people looking these up. So we invite comments…”
Sounds almost cosy. But if NCHS does rubber stamp the addition of Somatic symptom disorder to ICD-10-CM, it could leverage future replacement of the existing Somatoform disorders categories with this new, single diagnostic construct, bringing ICD-10-CM’s framework in line with DSM-5.
There are implications for ICD-11, too.
Once SSD is inserted into ICD-10-CM, the presence of this term within the U.S. modification of ICD-10 may make it easier for ICD-11 Revision Steering Group to justify approving proposals to replace the existing ICD-10 Somatoform disorders categories with a single, new disorder construct that would mirror SSD’s defining characteristics – its positive psychobehavioural features, its simplified criteria, its de-emphasis on “medically unexplained” – and facilitate harmonization between ICD-11 and DSM-5 disorder terms.
Christopher Chute, Mayo, chairs the ICD-11 Revision Steering Group. Chute has suggested that following implementation, ICD-10-CM might be brought gradually in line with ICD-11 through a series of annual updates, for smoother transition to ICD-11-CM.
Inserting the SSD term into ICD-10-CM paves the way for disorder construct congruency between DSM-5, ICD-10-CM, ICD-11, and eventually, the ICD-11-CM modification.
Send comments, by email, by June 20, to NCHS at nchsicd9CM@cdc.gov
CMS posts files for ICD-10-CM Release for 2015
On May 15, CMS posted the ICD-10 Procedure Coding System (ICD-10-PCS) files for 2015, download files here:
http://www.cms.gov/Medicare/Coding/ICD10/2015-ICD-10-PCS-and-GEMs.html
On May 19, CMS posted the ICD-10-CM and GEMs files for 2015:
http://www.cms.gov/Medicare/Coding/ICD10/2015-ICD-10-CM-and-GEMs.html
These files (some of which are large ZIP files) include:
2015 Code Descriptions in Tabular Order
2015 Code Tables and Index – Updated 5/22/14 (includes Tabular List, and Index in PDF format)
2015 ICD-10-CM Duplicate Code Numbers
2015 Addendum
2015 General Equivalence Mappings (GEMs) – Diagnosis Codes and Guide
2015 Reimbursement Mappings – Diagnosis Codes and Guide
According to the Addendum, “There were no changes to the 2014 ICD-10-CM, therefore there are no 2015 ICD-10-CM Addenda.”
These ICD-10-CM Release for 2015 files are not yet available on the CDC site but when they are posted, they should be accessible from this page: http://www.cdc.gov/nchs/icd/icd10cm.htm
Further reading