Round-up: Recent commentaries by Allen Frances, MD, on a DSM-5 in distress
February 22, 2012
Round-up: Recent commentaries by Allen Frances, MD, on a DSM-5 in distress
Post #146 Shortlink: http://wp.me/pKrrB-1X2
Allen Frances’ Blog at Huffington Post
DSM 5 Freezes Out Its Stakeholders
Allen Frances, MD | February 21, 2012
Scary news. The Chair of the DSM 5 Task Force, Dr. David Kupfer, has indicated that 90 percent of the decisions on DSM 5 have already been made.
Why so scary? DSM 5 is the new revision of the psychiatric diagnosis manual, meant to become official in May 2013. It proposes a radical redefinition of the boundary between mental disorder and normality, greatly expanding the former at the expense of the latter. Understandably, this ambitious medicalization of the human condition has generated unprecedented opposition, both from the public and from mental heath professionals. To top it off, the DSM 5 proposals are poorly written, unreliable, and likely to cause the misdiagnosis and the excessive treatment of millions of people.
Under normal circumstances the DSM 5 team would have taken the many criticisms to heart, gone back to the drawing board, and improved the quality and acceptability of their product. After all, the customer is very often right. But this DSM process has been strangely secretive, unable to self-correct, and stubbornly closed to suggestions coming from outside. As a result, current DSM 5 proposals show very little improvement over poorly done first drafts posted in February 2010.
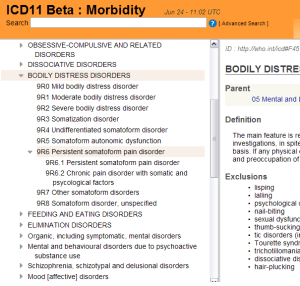
Is there any hope of a last-minute save? I have gathered opinions from three well-informed DSM 5 watchers. They were asked to assess the current state of DSM 5 and offer suggestions about future prospects. The first comment comes from Suzy Chapman, a public advocate, whose website provides the most comprehensive documentary source on the development of DSM 5 and ICD-11. Ms Chapman writes:
DSM 5 consistently misses every one of its deadlines and then fails to update its website with a new schedule. The Timeline was finally revised a couple of weeks ago, but we are still no nearer to a firm date for the final period of invited public comment. We’ve known since November that DSM 5 is stuffed as far as its planned January-February comment period and that Dr Kupfer now reckons “no later than May” – but all the website says is “Spring.” That’s no use to those of us who need to alert patient groups and their professional advisers…
DSM5 in Distress
The DSM’s impact on mental health practice and research.
by Allen Frances, M.D.Allen Frances, MD | February 22, 2012
Until yesterday, there were only two reasons to stick with the projected date of DSM 5 publication (May 2013): 1) the need to coordinate DSM 5 with ICD-10-CM coding, which was scheduled to start Oct 2013; and, 2) the need to protect APA publishing profits in order to meet budget projections.
The first reason just dropped out. Health and Human Services (HHS) Secretary Kathleen G. Sebelius has announced that the start date for ICD-10-CM has been postponed. It is not yet clear for how long, but most likely a year (see http://www.dhhs.gov/news/press/2012pres/02/20120216a.html ).
also on Psychiatric Times
Registration required for access
ICD-10-CM Delay Removes Excuse For Rushing DSM-5 Into Premature Publication
and Education Update
DSM 5 to the Barricades on Grief
Defending The Indefensible
Allen Frances, MD | February 18, 2012
The storm of opposition to DSM 5 is now focused on its silly and unnecessary proposal to medicalize grief. DSM 5 would encourage the diagnosis of ‘Major Depressive Disorder’ almost immediately after the loss of a loved one—having just 2 weeks of sadness and loss of interest along with reduced appetite, sleep, and energy would earn the MDD label (and all too often an unnecessary and potentially harmful pill treatment). This makes no sense. To paraphrase Voltaire, normal grief is not ‘Major’, is not ‘Depressive,’ and is not ‘Disorder.’ Grief is the normal and necessary human reaction to love and loss, not some phony disease.
All this seems perfectly clear to just about everyone in the world except the small group of people working on DSM 5. The press is now filled with scores of shocked articles stimulated by two damning editorial pieces in the Lancet and a recent prominent article in the New York Times.
The role of public defender of DSM 5 has fallen on John Oldham MD, president of the American Psychiatric Association…
Allen Frances, MD | February 17, 2012
Lancet Rejects Grief As a Mental Disorder: Will DSM 5 Finally Drop This Terrible Idea
The Lancet is probably the most prestigious medical journal in the world. When it speaks, people listen. The New York Times is probably the most prestigious newspaper in the world. Again, when it speaks, people usually listen. The Lancet and The New York Times have both spoken on the DSM-5 foolishness of turning grief into a mental disorder. Will DSM-5 finally listen?
Here are some selected quotes from today’s wonderful Lancet editorial
http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(12)60248-7/fulltextPrevious DSM editions have highlighted the need to consider, and usually exclude, bereavement before diagnosis of a major depressive disorder. In the draft version of DSM-5 , however, there is no such exclusion for bereavement, which means that feelings of deep sadness, loss, sleeplessness, crying, inability to concentrate, tiredness, and no appetite, which continue for more than 2 weeks after the death of a loved one, could be diagnosed as depression, rather than as a normal grief reaction.”
“Medicalising grief, so that treatment is legitimized routinely with antidepressants, for example, is not only dangerously simplistic, but also flawed…”
DSM 5 Minor Neurocognitive Disorder: Let’s Wait For Accurate Biological Tests
Allen Frances, MD | February 16, 2012
Within the next 3-5 years, we will likely have biological tests to accurately diagnose the prodrome of Alzheimer’s disease (AD). Much remains to be done in standardizing these tests, determining their appropriate set points and patterns of results, and negotiating the difficult transition from research to general clinical practice. And, given the lack of effective treatment, there are legitimate concerns about the advisability of testing for the individual patient and the enormous societal expense with little tangible benefit. Despite these necessary caveats, there is no doubt that biological testing for prodromal AD will be an important milestone in the clinical application of neuroscience.
How does this impact on the DSM 5 proposal to include a Minor Neurocognitive Disorder as a presumed prodrome to AD…
PTSD, DSM 5, and Forensic Misuse: DSM 5 would lead to overdiagnosis in legal cases.
Allen Frances, MD | February 09, 2012
In preparing DSM IV, we worked hard to avoid causing confusion in forensic settings. Realizing that lawyers read documents in their own special way, we had a panel of forensic psychiatrists go over every word to reduce the risks that DSM IV could be misused in the courts. They did an excellent job, but all of us missed one seemingly small mistake– the substitution of an ‘or’ for an ‘and’ in the paraphilia section that lead to serious misunderstandings and the questionably constitutional preventive psychiatric detention of sexual offenders.
DSM 5 is about to make a very different, less crucial, but still consequential forensic mistake. The proposed A criterion for PTSD includes the following wording…
Documentation That DSM 5 Publication Must Be Delayed because DSM 5 is so far behind schedule
Allen Frances, MD | February 07, 2012
I wrote last week that DSM 5 is so far behind schedule it can’t possibly produce a usable document in time for its planned publication date in May 2013. My blog stimulated two interesting responses that illustrate the stark contrast between DSM 5 fantasy and DSM 5 reality. Together they document just how far behind its schedule DSM 5 has fallen and illustrate why publication must be delayed if things are to be set right.
The first email came from Suzy Chapman of https://dxrevisionwatch.wordpress.com …
also on Psychiatric Times
Registration required for access
Additional coverage of DSM-5 controversies
Sidney Morning Herald
About-turn on treatment of the young
Amy Corderoy | February 20, 2012
CONCERNS about the overmedication of young people and rigid models of diagnosis have led the architect of early intervention in Australian psychiatry, Patrick McGorry, to abandon the idea pre-psychosis should be listed as a new psychiatric disorder.
The former Australian of the Year had previously accepted the inclusion of pre-psychosis – a concept he and colleagues developed – in the international diagnostic manual of mental disorders, or DSM, which is being updated this year.
Professor McGorry has been part of a team researching pre- and early-psychosis, and his work in the latter helped secure a massive $222.4 million Commonwealth funding injection for Early Psychosis Prevention and Intervention Centres across Australia…
Sidney Morning Herald
Suffer the children under new rules
Kathryn Wicks | Opinion | February 20, 2012
Canberra Times
A new chapter for psychiatrists’ bible
Amy Corderoy | February 19, 2012
Madness is being redesigned. The Diagnostic and Statistical Manual of Mental Disorders (DSM) will be updated this year, meaning what counts as a psychiatric disorder will change.
Frances, one of the architects of the current manual, DSM-IV, published in 1994, knows the results of his changes to the definitions of mental illness.
“We were definitely modest, conservative and non-ambitious in our approach to DSM-IV,” he says. “Yet we had three epidemics on our watch…”