Welcome to DSM-5 Facts (The APA’s new PR site)
May 31, 2012
Welcome to DSM-5 Facts (The APA’s new PR site)
Post #175 Shortlink: http://wp.me/pKrrB-2cm
There’s just a couple of weeks left until the deadline for receipt of stakeholder comments in the third and final review of DSM-5 proposals but still no sign of the promised “full results of the field trials” from the Task Force.
In the meantime, something else from the APA, or rather its PR firm. A spanking new DSM-5 Facts site launched this week “to correct the record” and provide the public with “a complete and accurate view of this important issue.”
Welcome to DSM-5 Facts
The American Psychiatric Association believes strongly in the work that is being done to revise the Diagnostic and Statistical Manual of Mental Disorders (DSM). In preparation for the release of DSM-5, experts from psychiatry, psychology, social work, neuroscience, pediatrics and other fields have committed much of the last five years to reviewing scientific research and clinical data, analyzing the findings of extensive field trials and reviewing thousand of comments from the public.
We welcome scrutiny, not only of this process but of its results.
Regrettably, news reports and commentators alike are filling the discourse with inaccurate, biased or misinformed criticism of DSM-5. Such information undermines the important changes that are being made to the manual, and provokes unwarranted confusion and fear among the individuals and families who stand to benefit most from essential care based on the strongest available diagnostic criteria.
The APA has created this forum to ensure observers of the DSM-5 development process have the facts.
Posted below are recent news stories, articles and opinion pieces, along with our responses, to correct the record, highlight key omissions — and provide essential perspective so that the public has a complete and accurate view of this important issue….
On the DSM-5 Facts Issue Accuracy page you’ll find responses to recent articles and Op-Eds by Allen Frances, Paula Caplan, NYT journalist, Benedict Carey, and Cosgrove and Krimsky.
In a counterpoint to Frances’ May 12, New York Times Op-Ed piece, APA responds:
APA Responds to Allen Frances New York Times Op-Ed
…There are actually relatively few substantial changes to draft disorder criteria. Those that have been recommended are based on the scientific and clinical evidence amassed over the past 20 years and then are subject to multiple review processes within the APA.
Unfortunately there is no comment facility on this DSM-5 Fact site.
One section for which substantial changes to disorder criteria are being proposed is the Somatoform Disorders.
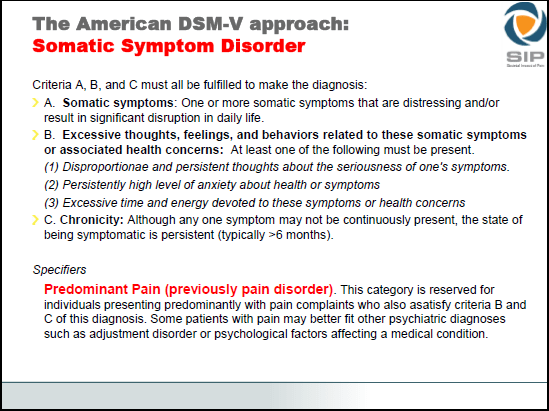
The Somatic Symptom Disorder Work Group proposes radical changes to this category: to rename the Somatoform Disorders section to “Somatic Symptom Disorders”; eliminate four existing DSM-IV categories: somatization disorder, hypochondriasis, pain disorder, and undifferentiated somatoform disorder; replace these discrete categories and their criteria with a single new category – “[Complex] Somatic Symptom Disorder” and apply new criteria.
“…To receive a diagnosis of complex somatic symptom disorder, patients must complain of at least one somatic symptom that is distressing and/or disruptive of their daily lives. Also, patients must have at least two [Ed: now reduced to “at least one from the B type criteria” since evaluation of the CSSD field trials] of the following emotional/cognitive/behavioral disturbances: high levels of health anxiety, disproportionate and persistent concerns about the medical seriousness of the symptom(s), and an excessive amount of time and energy devoted to the symptoms and health concerns. Finally, the symptoms and related concerns must have lasted for at least six months.
“Future research will examine the epidemiology, clinical characteristics, or treatment of complex somatic symptom disorder as there is no published research on this diagnostic category.”
“…Just as for complex somatic symptom disorder, there is no published research on the epidemiology, clinical characteristics, or treatment of simple somatic symptom disorder.”
And from the SSD Work Group Rationale/Validity Document (as published on May 4, 2011 for the second public review of draft proposals but not revised or reissued for the third review):
“…The presence of CSSD complicates management of all disorders and must be addressed in the treatment plan.
“It is unclear how these changes would affect the base rate of disorders now recognized as somatoform disorders. One might conclude that the rate of diagnosis of CSSD would fall, particularly if some disorders previously diagnosed as somatoform were now diagnosed elsewhere (such as adjustment disorder). On the other hand, there are also considerable data to suggest that physicians actively avoid using the older 6 diagnoses because they find them confusing or pejorative. So, with the CSSD classification, there may be an increase in diagnosis.
“The B-type criteria are crucial for a diagnosis of CSSD. These criteria in essence reflect disturbance in thoughts, feelings, and/or behaviors in conjunction with long standing distressing somatic symptoms. Whilst an exact threshold is perhaps arbitrary, considerable work suggests that the degree of functional impairment is associated with the number of such criteria. Using a threshold of 2 or more such criteria results in prevalence estimates of XXXX in the general population, XXXX in patients with known medical illnesses, and XXXX in patients who may previously have been considered to suffer from a somatoform illness. {text in development concerning impact of different thresholds for criteria B- from Francis [Creed]}…”
No data on prevalence estimates available for the second review and no data on impact of different thresholds for the B type criteria and prevalence estimates available for the third review.
I will update if a report on the field trials is released.
Commentary from Allen Frances on the launch of this new DSM-5 Fact site.
Huffington Post Blogs | Allen Frances
Public Relations Fictions Trying to Hide DSM 5 Facts
Allen Frances MD | May 31, 2012
Recently APA recruited a public relations guy from the Department of Defense to respond to my concerns that DSM 5 is way off track. He immediately went on the offensive and (in an interview for Time magazine) made the obvious PR mistake of calling me “a dangerous man.” This provided me the opportunity to pose yet again the troubling questions about DSM 5 that APA repeatedly refuses to answer. The DOD guy hasn’t surfaced since.
Instead, APA has adopted a much smoother, soft sell approach. It has hired GYMR — an expensive PR firm. GYMR actually brags in its mission statement that it can “execute strategies that include image and alliance building, public education campaigns or media relations to harness the formidable forces of Washington and produce successful results for clients.”
We now have the first fruits of GYMR’s “image building” misinformation campaign. It has launched a PR website with the claim it will provide “the facts on DSM-5 development process. Read recent news stories & opinion pieces, along with our responses, to correct the record, highlight key omissions — and provide essential perspective, so that the public has a complete and accurate view of this important issue.”
Unfortunately, the site is very short on accurate facts, very long on misleading (or just plain wrong) “image building” fiction. It is all pure PR fluff — a way to avoid answering the substantive questions that need addressing before DSM 5 is prematurely rushed to press. Let’s compare GYMR fiction versus DSM 5 fact:
GYMR Fiction: “We have extensive data from the field trials that on average there is a slight decrease in the overall rates of DSM-5 in comparison to DSM-IV disorders.”
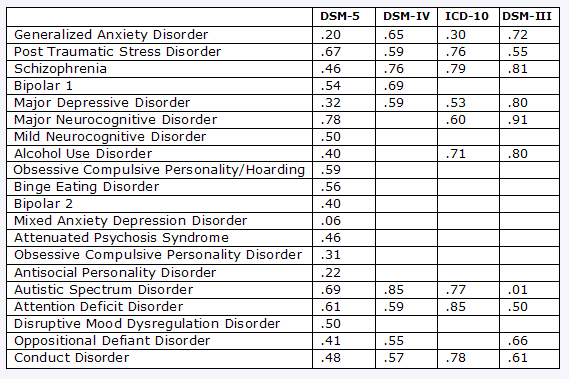
DSM 5 Fact: This is simply wrong — APA has no such data. Except for autism, all of the DSM 5 changes will dramatically raise the rates of mental disorder and mislabel normal people as psychiatrically sick. The field trial provided no data on this crucial question because it made an unforgivable error — not including head to head prevalence comparisons between DSM IV and DSM 5. This makes it impossible to estimate how explosive will be the DSM 5 rate jumps. Moreover, false epidemics are often nurtured in the primary care settings that were untested in the DSM 5 field trials.
GYMR Fiction: The PR claim is that DSM 5 has provided a transparent process.
DSM 5 Fact: DSM 5 has been peculiarly and self-destructively secretive from its early confidentiality agreements (meant to protect intellectual property) to its current failure to make public any of the results of its ‘scientific’ reviews. Real science can never be confidential. None of this secrecy makes any sense.
GYMR Fiction: “APA takes very seriously its responsibility in developing and maintaining DSM and has devoted $25 million to the DSM-5 update process thus far.”
DSM 5 Fact: The $25 million has been a colossal waste of poorly spent money. We did DSM IV for one-fifth the price and never missed a deadline or stirred much controversy. The difference in expenditure and outcome has nothing to do with us being especially competent. It has everything to do with DSM 5 being poorly conceived and organized and spending lavishly on silly things like public relations.
GYMR Fiction: “There are several proposals in DSM-5 that aim to more accurately describe the symptoms and behaviors of disorders that typically present in children.”
DSM 5 Fact: The epidemics of excessive diagnosis in children will be muddled further by DSM 5. The threshold for ADHD is being lowered despite the tripling of rates. Temper Dyregulation (AKA DMDD) is being suggested based on just a few years of work by just one research group — despite the risk it will exacerbate the already inappropriate and dangerous use of antipsychotic drugs in kids. And DSM 5 somehow persists in not understanding how its suggestions will necessarily have a profound impact on rates of autism.
GYMR Fiction: “There are actually relatively few substantial changes to draft disorder criteria.”
DSM 5 Fact: Dead wrong — how did GYMR ever come up with this one? My guess is that the DSM 5 changes would affect the diagnosis of tens of millions of people. APA has no way of refuting this estimate since it unaccountably failed to ask the crucial prevalence question in its $3 million field trial.
GYMR Fiction: “Those that have been recommended are based on the scientific and clinical evidence amassed over the past 20 years and then are subject to multiple review processes within the APA.”
DSM 5 Fact: Most of the reviews are poorly done and none of the suggestions would stand up to the kind of impartial, independent scientific review demanded by a petition supported by 51 mental health associations. The APA internal review lacks any credibility because it is done in secret and has somehow found a way to approve DMDD and the removal of the bereavement exclusion — both of which have little or no scientific support. To be credible, APA must both make public its own scientific reviews and also contract for external and independent reviews on all the most controversial topics.
GYMR Fiction: “The APA governance attention to this is far greater than anything that ever occurred with DSM III or DSM-IV.”
DSM 5 Fact: Absurd on the face of it. If there had ever been anything resembling proper internal supervision, DSM 5 would not be in this deep mess and would not require expensive PR fig leaves to try to cover it up.
There is more, but you get the idea. DSM 5 is in a paradoxical position. Publishing profits pressure it toward premature publication, but its close to final draft is the object of almost universal opposition. On one side we have APA and its new hired gun GYMR — on the other side we have 51 professional organizations, the Lancet, the New England Journal of Medicine, the international media and outraged segments of the public. It is far too late for any superficial “image building,” however clever, to restore DSM 5 credibility. Saving DSM 5 requires radically reforming its mistakes, not covering them up with a PR smokescreen of misinformation.
The last and only hope for a safe and credible DSM 5 now resides in the new APA leadership — it is within its power to thoroughly reform DSM 5 before it is too late.
The stakes are high. A DSM 5 at war with its users will wind up losing many of them. Disillusioned members (each of whom has involuntarily sunk almost $1,000 in this lavish but misdirected DSM 5 effort) will speed up the already rapid exodus of APA members. APA will eventually lose its monopoly on psychiatric diagnosis. Psychiatry will be unfairly discredited. And, worst of all, the patients who need our help will suffer.
DSM 5 is in such public trouble now because it heedlessly missed every prior private opportunity to self-correct. The solution is not the production of more public relations pablum. Instead, DSM 5 needs to regroup, solve its problems, and avoid racing over a cliff.