January 29, 2014
by admindxrw
Update on February 2, 2014:
Since publishing my report, below, the Chapter 5 parent class:
“Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere”
has been reverted by ICD-11 Revision to read, “Bodily distress disorders”.
The category, 5C70 Psychological and behavioural factors associated with disorders or diseases classified elsewhere [F54 in ICD-10], which had been, and remains listed as an Exclusion to class “Bodily distress disorders”, is now coded towards the end of the list of Chapter 5 Mental and behavioural disorders categories, rather than listed as a hierarchical child category under:
“Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere”.
Note that the Definition and Inclusions for “5C70 Psychological and behavioural factors associated with disorders or diseases classified elsewhere” are legacy text carried over from ICD-10. The Fxx codes listed under “Exclusions” for this category have not yet been updated to reflect the new ICD-11 coding structure.
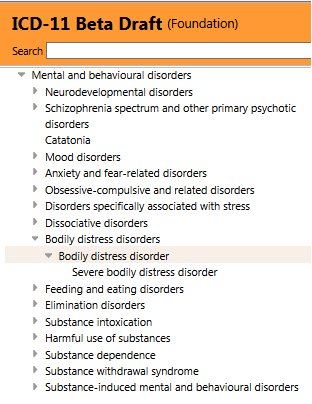
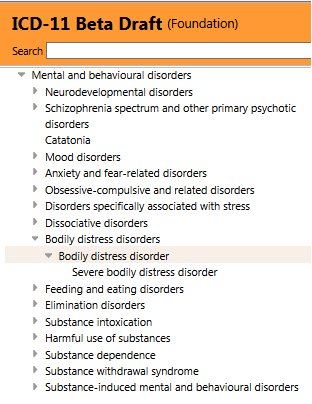
This section of Chapter 5 now displays as in this screenshot, immediately below, when viewed in the ICD-11 Beta drafting platform Foundation View, at February, 2, 2014:
http://apps.who.int/classifications/icd11/browse/f/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f1472866636
A change also for Hypochondriasis – which has also been removed from under parent class, Bodily distress disorders, and is currently assigned dual parentage under: Obsessive-compulsive and related disorders; and Anxiety and fear-related disorders.
This means that the only categories currently coded under parent term “Bodily distress disorders” (previously, “Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere”) are “Bodily distress disorder” and “Severe bodily distress disorder“.
Update on February 1, 2014:
In June 2013, Prof David Goldberg co-authored a paper: Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (MUS) in Mental Health in Family Medicine. Co-author, Gabriel Ivbijaro, is Editor in Chief, Mental Health in Family Medicine and a past Chair of the Wonca Working Party on Mental Health. Mental Health in Family Medicine is the official journal of The World Organization of Family Doctors (Wonca) Working Party on Mental Health. I don’t have access to this paper, which is currently embargoed, but it should be free in PMC on June 1, 2014 [5].
+++
Screenshot: Chapter 5, ICD-11 Beta drafting platform, public version: January 29, 2014
+++
Between a Rock and a Hard Place
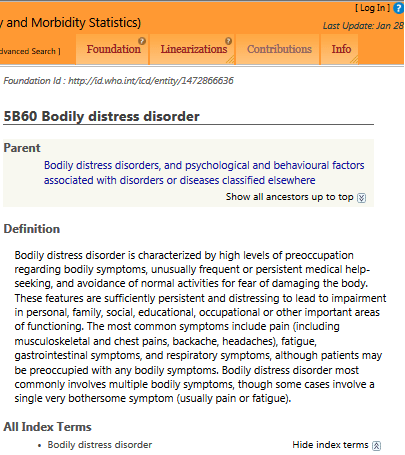
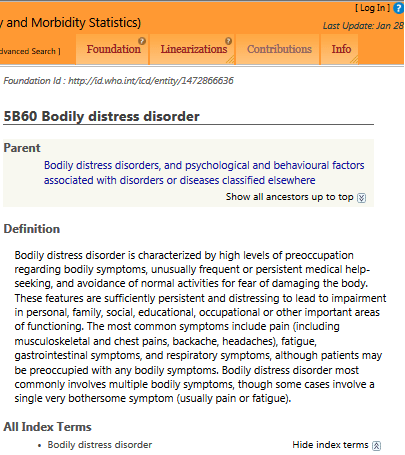
A definition for “Bodily distress disorder” has very recently been entered into the public version of the ICD-11 Beta drafting platform by ICD-11 Revision.
You can view the definition text, as it stands at January 29, in the public version of the Beta drafting platform, here:
Joint Linearization for Mortality and Morbidity Statistics view
Bodily distress disorder
Parent(s)
Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere
Definition
Bodily distress disorder is characterized by high levels of preoccupation regarding bodily symptoms, unusually frequent or persistent medical help-seeking, and avoidance of normal activities for fear of damaging the body. These features are sufficiently persistent and distressing to lead to impairment in personal, family, social, educational, occupational or other important areas of functioning. The most common symptoms include pain (including musculoskeletal and chest pains, backache, headaches), fatigue, gastrointestinal symptoms, and respiratory symptoms, although patients may be preoccupied with any bodily symptoms. Bodily distress disorder most commonly involves multiple bodily symptoms, though some cases involve a single very bothersome symptom (usually pain or fatigue).
All Index Terms
Or here, in the Beta Foundation view
—————-
Only the ICD-11 Short (100 word) Definition for this proposed new ICD category has been inserted. At this point, no Inclusion Terms, Exclusions, Synonyms, Narrower Terms, Diagnostic Criteria or other potential Content Model descriptors have been populated.
No Definition or severity characteristics have yet been assigned to Severe bodily distress disorder to differentiate between the two coded severities: “Bodily distress disorder” and “Severe bodily distress disorder.” (Unique codes for a “Mild bodily distress disorder” and a “Moderate bodily distress disorder” were dropped in mid 2013.)
In order to place this development into context here are some notes:
It’s important to understand that there are two working groups reporting to the International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders that are charged with making recommendations on the revision of the Somatoform Disorders for the primary care version and core version of ICD-11:
The 12 member Primary Care Consultation Group (PCCG) leads the development and field testing of the revision of all 28 mental and behavioural disorders for inclusion in the next ICD primary care classification (ICD-11-PHC), an abridged version of the core ICD classification. The PCCG is chaired by Prof Sir David Goldberg. Per Fink’s colleague, Marianne Rosendal, is a member of this group.
The 17 member Expert Working Group on Somatic Distress and Dissociative Disorders (S3DWG) is advising on the revision of ICD-10’s Somatoform Disorders. The S3DWG is chaired by Prof Oye Gureje. DSM-5 Somatic Symptom Disorder work group member, Prof Francis Creed, is a member of this group.
In 2011, the Primary Care Consultation Group’s proposals for a replacement for the “Unexplained somatic symptoms/medically unexplained symptoms” category were put out for review and evaluation in primary care settings to nine international focus groups* in seven countries [1].
*Austria, Brazil, Hong Kong, New Zealand, Pakistan, Tanzania and United Kingdom.
The PCCG anticipated refining their recommendations in the light of focus group responses before progressing to field testing the new disorder.
New disorders that survive the primary care field tests must have an equivalent disorder in the main ICD-11 classification.
Since any new primary care disorder concept will need to integrate into the ICD-11 core version, one might expect some cross-group collaboration between these two advisory committees.
But in their respective 2012 journal papers, the groups presented divergent constructs and neither group refers to the work being undertaken by the other group, or sets out how the two groups relate to each other, or how the primary care group relates to the overall revision process for the Somatoform Disorders.
The specific tasks of the S3DWG include, among others:
“3. To provide drafts of the content (e.g. definitions, descriptions, diagnostic guidelines) for somatic distress and dissociative disorder categories in line with the overall ICD revision requirements.
“4. To propose entities and descriptions that are needed for classification of somatic distress and dissociative disorders in different types of primary care settings, particularly in low- and middle-income countries.”
It is unclear how ICD-11 Revision is co-ordinating the input from the two groups, that is, will it be the PCCG’s revised recommendations that progress to field testing, this year, and if so, how would a divergent set of proposals, developed in parallel by the S3DWG group, relate to the field testing and to the overall revision of the SDs?
Or, will ICD-11 Revision require the PCCG group and the S3DWG group to agree on what to call any proposed, single disorder replacement for six or seven SD categories and to reach consensus over what construct, definition, characteristics and criteria will go forward to ICD-11 field testing, and if so, has consensus now been reached?
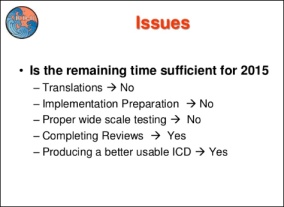
Field tests are expected to start this year. Currently, there is no publicly available information on the finalized characteristics, diagnostic guidelines, criteria, inclusions, exclusions, differential diagnoses etc. that are planned to be used for the field tests which would provide the level of detail lacking in this Beta draft definition.
It has been crafted with sufficient elasticity to allow either group’s construct to be shoehorned into it.
ICD-11 Revision is possibly hedging its bets depending on the outcome of its field tests. But the devil’s in the detail and without the detail, it isn’t clear whether this definition describes the construct favoured by the S3DWG in late 2012, or by the PCCG in mid 2012, or a more recent revision by one of the groups, or a compromise between the two.
The definition wording is based – in some places verbatim – on the construct descriptions presented in the Gureje, Creed (S3DWG) “Emerging themes…” paper, published in late 2012 [2].
Extract, Creed F, Gureje O. Emerging themes in the revision of the classification of somatoform disorders. Int Rev Psychiatry. 2012:
“…At the time of preparing this review, a major highlight of the proposals of the S3DWG for the revision of the ICD-10 somatoform disorders is that of subsuming all of the ICD-10 categories of F45.0 – F45.9 and F48.0 under a single category with a new name of ‘bodily distress disorder’ (BDD).
“In the proposal, BDD is defined as ‘A disorder characterized by high levels of preoccupation related to bodily symptoms or fear of having a physical illness with associated distress and impairment. The features include preoccupation with bothersome bodily symptoms and their significance, persistent fears of having or developing a serious illness or unreasonable conviction of having an undetected physical illness, unusually frequent or persistent medical help-seeking and avoidance of normal activities for fear of damaging the body. These features are sufficiently persistent and distressing to lead to impairment of functioning or frequent seeking of reassurance.'”
This 2012 paper goes on to say that the S3DWG’s emerging proposals specify a much simplified set of criteria for a diagnosis of Bodily distress disorder (BDD) that requires the presence of: 1. High levels of preoccupation with a persistent and bothersome bodily symptom or symptoms; or unreasonable fear, or conviction, of having an undetected physical illness; plus 2. The bodily symptom(s) or fears about illness are distressing and are associated with impairment of functioning.
And that in doing away with the “unreliable assumption of its causality” the diagnosis of BDD does not exclude the presence of depression or anxiety, or of a co-occurring physical health condition.
Which is a disorder construct into which DSM-5’s “Somatic Symptom Disorder” (SSD) could be integrated, thus facilitating harmonization between ICD-11 and DSM-5.
But without clarification from ICD-11 Revision (or further published papers, reports or sight of the field test protocol) I do not think one can safely extrapolate that it is the current proposals of the S3DWG group that are going forward to field testing, this year, in preference to a construct and criteria favoured by the PCCG group.
With the caveat that proposals by both groups are likely to have been modified since publication of their respective 2012 papers, or may have since converged into a consensus concept, to recap briefly:
In mid 2012, the Goldberg led PCCG primary care group was proposing a new term called “Bodily stress syndrome (BSS),” to replace ICD’s primary care category, “F45 Unexplained somatic symptoms.” This single BSS category would also absorb F48 Neurasthenia, which is proposed to be eliminated for ICD-11-PHC.
In late 2012, the S3DWG group was proposing to subsume the six ICD-10 categories F45.0 – F45.9, plus F48.0 Neurasthenia, under a single disorder category, but under the disorder name, “Bodily distress disorder” (BDD).
So at that point, the two groups differed on what term should be used for this new disorder.
The two group’s proposed constructs, criteria and exclusions also diverged, with the PCCG group incorporating characteristics of Fink et al’s “Bodily Distress Syndrome” [3] construct, and based on the “autonomic arousal” (or “over-arousal”) illness model, with symptom clusters or symptom patterns from one or more body systems, but also requiring some SSD-like psychobehavioural responses to meet the diagnosis. But, “If the symptoms are accounted for by a known physical disease this is not BSS.”
While the emerging proposals of the S3DWG group leaned more towards a “pure” DSM-5 SSD-like construct that could be diagnosed in patients with persistent “excessive” psychobehavioural responses to bodily symptoms in the presence of any diagnosed disease, patients with so-called “functional somatic syndromes” and patients with somatic symptoms of unclear etiology, but with no evident requirement for specific symptom counts, or for symptom clusters from one or more body systems or for the symptoms to be “medically unexplained.” [4]
What wasn’t explicitly set out in the PCCG’s 2012 paper was whether the group intended to mirror the Fink et al BDS construct to the extent of extending the diagnosis to be inclusive of the so-called “functional somatic syndromes,” FM, CFS and IBS (which are currently discretely coded or indexed within ICD-10 in chapters outside the mental and behavioural disorders chapter).
This 2013 paper, below, interprets that it is the intention of the Primary Care Consultation Group to capture FM, CFS and IBS:
http://www.ncbi.nlm.nih.gov/pubmed/24295235
Free PDF: http://www.uam.es/becarios/jbarrada/papers/hads.pdf
Psychol Assess. 2013 Dec 2. [Epub ahead of print] Bifactor Analysis and Construct Validity of the HADS: A Cross-Sectional and Longitudinal Study in Fibromyalgia Patients. Luciano JV, Barrada JR, Aguado J, Osma J, García-Campayo J.
“[…] In the upcoming primary healthcare version of the ICD-11 (ICD-11-PHC), FM will be classified as part of bodily stress syndrome (BSS; Lam et al., 2013). This new diagnosis will group patients who might have previously been considered different (e.g., those with FM, chronic fatigue syndrome, irritable bowel syndrome, and so on). Frontline clinicians (e.g., GPs) will need reliable tools to identify possible/probable clinical cases of anxiety (i.e., cognitive over-arousal) among patients with BSS who are characterised by elevated somatic over-arousal…”
Prof Tony Dowell, New Zealand, is a member of the PPCG. In this slide presentation Prof Dowell lists IBS, Fibromylagia and CFS under “Bodily Stress Syndromes.” Prof Dowell is already promoting the use of the BSS construct, in New Zealand, despite its current lack of validation:
Slide presentation
Slide 29
Bodily Stress Syndromes
• Gastroenterology – IBS, Non ulcer dyspepsia
• Rheumatology – Fibromyalgia
• Cardiology – Non cardiac chest pain
• Respiratory – hyperventilation
• Dental – TMJ syndrome
• Neurology – ‘headache’
• Gynaecology – chronic pelvic pain
• Psychiatry – somatiform [sic] disorders
• Chronic fatigue Syndrome
Reading the responses of the focus groups, as reported in the Lam et al paper [1], it is evident that some focus group participants understood the proposed BSS construct as a diagnosis under which IBS, Fibromylagia and CFS patients could potentially be assigned; though one of the New Zealand focus groups noted there was quite a strong feeling that CFS did not fit the paradigm as well as other [FSS] disorders, particularly when there was a good history of preceding viral infection.
Whilst a number of diseases are listed in the PCCG criteria, as proposed in 2012, under “Differential diagnoses,” including multiple sclerosis, hyperparathyroidism, systemic lupus erythematosus and Lyme disease – IBS, Fibromylagia, CFS and ME are omitted from the list of “Differential diagnoses” examples.
In June 2013, Prof David Goldberg co-authored a paper: Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (MUS) in Mental Health in Family Medicine. Co-author, Gabriel Ivbijaro, is Editor in Chief, Mental Health in Family Medicine and a past Chair of the Wonca Working Party on Mental Health. Mental Health in Family Medicine is the official journal of The World Organization of Family Doctors (Wonca) Working Party on Mental Health.
I don’t have access to this paper, which is currently embargoed, but it should be free in PMC on June 1, 2014 [5].
—————-
When viewing the Beta drafting platform, note that the descriptive text for the ICD-11 Beta draft parent term, “Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere,” which can be viewed here: ICD-11 Beta drafting platform Foundation view is the legacy text from the beginning of the ICD-10 Somatoform Disorders section (compare in ICD-10 here):
This F45 section introduction text has not yet been revised to reflect the proposed dismantling and reorganization of the ICD-10 Somatoform Disorders section for ICD-11.
Caveat: The ICD-11 Beta draft is not a static document – it is a work in progress, subject to daily revisions and refinements and to approval by the International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders, the ICD-11 Revision Steering Group, and WHO classification experts. Proposals for some new or revised disorders may be subject to re-evaluation and revision following ICD-11 field testing.
References:
1. Lam TP, Goldberg DP, Dowell AC, Fortes S, Mbatia JK, Minhas FA, Klinkman MS: Proposed new diagnoses of anxious depression and bodily stress syndrome in ICD-11-PHC: an international focus group study. Fam Pract Feb 2013 [Epub ahead of print July 2012]. http://www.ncbi.nlm.nih.gov/pubmed/22843638 [Full text behind paywall]
2. Creed F, Gureje O. Emerging themes in the revision of the classification of somatoform disorders. Int Rev Psychiatry. 2012 Dec;24(6):556-67. http://www.ncbi.nlm.nih.gov/pubmed/23244611 [Full text behind paywall]
3. Fink et al’s Bodily Distress Syndrome
Per Fink and colleagues are lobbying for their “Bodily Distress Syndrome” (BDS) construct to be integrated into forthcoming classification systems and adopted as a diagnosis by primary care practitioners. They propose the reclassification of the somatoform disorders, pain disorder, neurasthenia and the so-called functional somatic syndromes, including fibromyalgia (FM), irritable bowel syndrome (IBS) and chronic fatigue syndrome (CFS), under a single, unifying diagnosis, “Bodily Distress Syndrome,” already in use in clinical and research settings in Denmark.
4. BDS, BDDs, BSS, BDD unscrambled
5. Ivbijaro G, Goldberg D. Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (MUS). Ment Health Fam Med. 2013 Jun;10(2):63-4. No abstract available. [PMID: 24427171] Currently embargoed: Free in PMC on June 1, 2014. PMC Archives
G Ivbijaro is Editor in Chief, Mental Health in Family Medicine and a past Chair of the Wonca Working Party on Mental Health. D Goldberg chairs the Primary Care Consultation Group (PCCG) leading the development and field testing of the next ICD primary care classification (ICD-11-PHC).
6. General information on ICD-11 Field Tests:
2012 Annual Report of the International Union of Psychological Science to the American Psychological Association Revision of World Health Organization’s ICD-10 Mental and Behavioural Disorders, Pierre L.-J. Ritchie, Ph.D, January, 2013, Pages 8-11
Click to access icd-report-2012.pdf
WHO ICD Revision Information Note: Field Trials, 23 January 2013
Click to access 15.Field_Trials.pdf



 2013 All rights reserved. Current Biology,
2013 All rights reserved. Current Biology, 
Objectors to insertion of DSM-5’s Somatic symptom disorder into ICD-10-CM
November 16, 2013 by admindxrw
Post #283 Shortlink: http://wp.me/pKrrB-3y8
Michael Munoz, Executive Director, Rocky Mountain CFS/ME & FM Association has organized a joint letter of objection signed by 13 U.S. patient organizations and advocates for submission to NCHS. It can be read here:
http://www.rmcfa.org/index.html > http://www.rm-cfs-fms.citymaker.com/f/NCHS.pdf
or download PDF here: Joint response to NCHS 11.15.13
This joint submission had been signed by the following organizations and advocates:
I’d like to thank all those who have submitted objections to NCHS in opposition to the September 2013 C & M Committee meeting proposal to insert Somatic symptom disorder as an inclusion term in ICD-10-CM.
My submission can be read here PDF: Submission NCHS
Some additional organizations and individuals have advised me of their own submissions. If you have submitted a response on behalf of your organization or as a patient, advocate or professional and you would like your name or your organization’s name added to the list of responders below please shoot me an email or contact me via the Contact form with a link to your submission (if it has been placed in the public domain) and a couple of lines of credentials or stakeholder interest, if desired.
Share this:
Filed under American Psychiatric Association (APA), Darrel Regier, DSM-5, Functional Somatic Syndrome (FSS), ICD-10-CM, ICD-11, MUS, Myalgic encephalomyelitis, Somatic Symptom Disorder, Somatoform Disorders Tagged with american psychiatric association, dsm-5, functional somatic syndrome, icd-10-cm, icd-11, institute of psychiatry, NCHS, public comment, somatic symptom disorder, somatoform disorders