Proposals for the classification of Chronic pain in ICD-11: Part 2
August 22, 2015
Post #326 Shortlink: http://wp.me/pKrrB-48Y
Click here for Part 1
Note: Since these proposed changes for Fibromyalgia were published on the ICD-11 Beta draft, in 2015, not a single comment has been posted via the ICD-11 Comment or Proposals mechanisms from stakeholder patient organizations, the clinicians who advise them, allied health professionals or disability lawyers.
Part 2: Fibromyalgia
On May 5, 2015, the ICD-11 Beta draft category, Fibromyalgia, was deleted from the Diseases of the musculoskeletal system and connective tissue chapter and relocated under Symptoms, signs, clinical forms, and abnormal clinical and laboratory findings, not elsewhere classified (currently numbered Chapter 21 in the Beta draft).*
*Source: Fibromyalgia Change History, 05 May 2015
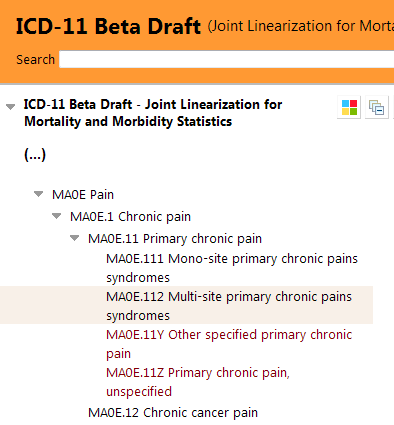
For ICD-11, Fibromyalgia is proposed to be listed under the Symptoms, signs chapter, under a proposed new parent category called Multi-site primary chronic pains syndromes, under new parent class, Chronic primary pain, under new parent class, Chronic pain.
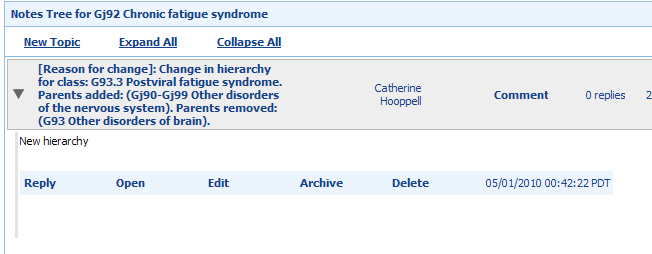
No rationale for a proposed change of chapter location and parent class was recorded in the Change History at the time of the edit.
See Part 1 and the June 2015 paper A classification of chronic pain for ICD-11. Rolf-Detlef Treede, Winfried Rief et al for the IASP working group’s proposals for locating irritable bowel syndrome; chronic nonspecific back pain; chronic pelvic pain; chronic widespread pain, fibromyalgia, and potentially some other conditions where chronic pain is a feature, under proposed new disorder category, Chronic primary pain.
Some of the categories listed under the new Chronic pain parent are proposed to be secondary parented (cross-referenced) to other chapters. But it is unclear from the proposals, whether Fibromyalgia is intended to be secondary parented to the Diseases of the musculoskeletal system and connective tissue chapter or to Diseases of the nervous system, or whether some disorders categorized under Chronic primary pain disorder would have no secondary parent chapter association beyond the Symptoms, signs chapter.
ICD-11 Beta Foundation Component
In the ICD-11 Foundation Component (where all ICD-11 entities are listed), Fibromyalgia is listed under Chronic pain > Primary chronic pain > Multi-site primary chronic pains syndromes, and assigned a Definition and other Content Model descriptors**.
View the Beta draft Foundation Component here: Fibromyalgia
**The current Beta draft Definitions for Fibromyalgia do not appear to have been revised from how the text had stood prior to its chapter relocation in May 2015.
(The likely source for the text entered into the Definition and Long Definition fields is this Orphanet page, apparently last updated in May 2007, but which appends links to more recent criteria and practice guidelines.)
From the ICD-11 Beta draft Foundation Component (accessed August 20, 2015):
Fibromyalgia

But in the Joint Linearization for Mortality and Morbidity Statistics (JLMMS), Fibromyalgia is not proposed to be listed with a discrete code assigned but rolled up as an Inclusion term under MAOE.112 Multi-site primary chronic pains syndromes.
View the Beta draft JLMMS linearization here: Fibromyalgia
This screenshot shows the hover text for Inclusion term, Fibromyalgia, in the JMMLS linearization:

ICD-11 Beta drafting platform, public version: Joint Linearization for Mortality and Morbidity Statistics. Accessed August 20, 2015.
I am not a stakeholder or advocate for Fibromyalgia or for any of the several terms proposed to be categorized under the Primary chronic pain/Chronic primary pain parent term.
Consideration of the implications for aggregating Fibromyalgia, chronic widespread pain, irritable bowel syndrome, chronic nonspecific back pain, chronic pelvic pain and some other conditions where chronic pain is a predominate feature, under a new term in the Symptoms, signs chapter, on data collection, research, commissioning of services, access to treatments, reimbursement etc. is beyond the scope of this report.
But I urge stakeholder patient organizations, the clinicians who advise them, allied health professionals, occupational therapists and disability lawyers to scrutinize the IASP Task Force paper, the Beta draft rationale and proposals documents, proposed definitions and other descriptive content and to register with the Beta draft to submit comments and make formal suggestions for improvements via the Proposal Mechanism, (supported with references, where possible).
There is a considerable amount of psychosomatics in the Detailed Proposals document for Primary chronic pain. There is disorder description and criteria overlap with ICD-11’s proposed Bodily distress disorder; with DSM-5 Somatic symptom disorder “Predominate pain” specifier; with Somatoform pain disorder and the German ICD-10-GM: F45.41: Chronic pain disorder with somatic and psychological factors – a classification which Prof Winfried Rief was instrumental in getting inserted into the German ICD-10-GM, in 2009.
Prof Winfried Rief slide presentation:
Back in 2012, Chronic pain Task Force co-chair, Prof Winfried Rief, had presented tentative ideas for potential frameworks for a new ICD-11 chapter or section for pain conditions:
2012 SIP Symposium Workshop presentation: IASP and the Classification of Pain in ICD-11
Note in Slides #12-15, a number of the so-called, functional somatic syndromes, and in Slide #15, “Chronic Fatigue Syndrome, Neurasthenia” [sic], had been floated by Prof Rief, in 2012, as potential partners in any proposed new chapter or section for chronic pain.
Key documents for scrutiny by patient organizations, clinicians and advocates
A classification of chronic pain for ICD-11 Treede R, Rief W, et al, June 2015
Detailed Rationale/proposals/criteria documents:
Chronic pain 2015-May-26 Antonia Barke
Chronic primary pain 2015-June-29 Antonia Barke
Chronic visceral pain 2015-May-26 Antonia Barke
Chronic musculoskeletal pain 2015-May-26 Antonia Barke
Current ICD-11 Beta draft location Foundation Component listing for Irritable bowel syndrome
ICD-11 Beta draft Foundation Component listing for Fibromyalgia
ICD-11 Beta draft JLMMS listing for Fibromyalgia [rolled up as Inclusion in Multi-site primary chronic pains syndromes]
Click here for Part 1
Further reading
Medscape article: Chronic Pain Syndrome, Manish K Singh, MD; Chief Editor: Stephen Kishner, MD, MHA, updated July 15 2015
The Changing Nature of Fibromyalgia. Frederick Wolfe and Brian Walitt