WHO Collaborating Centre confirms Revision Steering Group seriously considering extension to ICD-11 timeline
January 22, 2014
Post #289 Shortlink: http://wp.me/pKrrB-3E8
Update at January 30, 2014:
ICD-11 Revision has confirmed that a decision has now been taken to postpone ICD-11 by a further two years, from 2015 to 2017.
From WHO site: “The International Classification of Diseases 11th Revision is due by 2017”
Information in this report relates to the development of the World Health Organization’s ICD-11. It does not apply to the forthcoming US specific, NCHS developed, clinical modification of ICD-10, known as ICD-10-CM.
Source: Slide 34: Where are we? What remains to be done? Shall we have ICD WHA submission in 2015 or later? B Üstün, World Health Organization Classifications, Terminologies, Standards ICD Revision: Quality Safety Meeting, September 2013
The December newsletter of the WHO Collaborating Centre for the Family of International Classifications (FIC) in the Netherlands reports that ICD-11 Revision Steering Group (RSG) is reviewing options for a further extension to the ICD-11 development timeline [1]:
Newsletter on the WHO-FIC, Volume 11, Number 2, 2013, Latest News, Page 3 [PDF]
The Revision Steering Group and WHO Secretariat seriously consider amending the timeline of submitting the ICD-11 for endorsement by the World Health Assembly to allow more time for field testing in multiple countries and settings, and following up on resulting edits. WHO currently discusses options and scenarios with stakeholders.
This announcement from WHO-FIC’s Marijke de Kleijn-de Vrankrijker reinforces information and resources provided in my September report (WHO considers further extension to ICD-11 development timeline) – that ICD-11 Revision is failing to meet development targets and delaying submission of ICD-11 for WHA for approval until 2016, or alternatively, extending the timeline by a further two years, for WHA approval in 2017, is under consideration.
ICD-11 already four years behind original targets
The revision of ICD-10 and development of the structure for ICD-11 began in 2007. WHO’s original goal had been to complete the revision and release of ICD-11 by 2011-12, Archived documents [2] [3].
By 2009, the date for submission of ICD-11 for WHA approval had been extended to 2014. The launch of the public version of the Beta drafting platform was later postponed from May 2011 to May 2012.
The current projection for submission of ICD-11 for approval to WHA is May 2015, with dissemination in 2015+ [4].
Mayo’s Christopher Chute, MD, chairs the ICD-11 Revision Steering Group. According to Chute, in this paper published in March 2012, publication of ICD-11 is “expected around 2016″:
Chute CG, Huff SM, Ferguson JA, Walker JM, Halamka JD. There Are Important Reasons For Delaying Implementation Of The New ICD-10 Coding System. Health Aff March 2012 DOI: 10.1377/hlthaff.2011.1258
ICD Revision considers its options
In September, WHO posted this meeting materials document [5] and this slide presentation [6]. The document summarized, inter alia, ICD-11’s progress, current development status, timelines for finalization date and approval by WHO Governing Bodies, and rationales and options for a further shift in the timeline.
You can read extracts from the document and view slides setting out the options currently under consideration in this report: WHO considers further extension to ICD-11 development timeline, selected of which I am appending to this post.
The earliest ICD-11 might be ready for dissemination is late 2015/16 – which may require some further scaling back of the project’s goals.
But if ICD-11 Revision Steering Group does elect to postpone submission for World Health Assembly approval until May 2017, dissemination of ICD-11 may not be viable before 2018.
I will update this post if and when WHO or ICD-11 Revision Steering Group publish a statement of clarification on the WHO website or issue a news release, or if other information becomes available that confirms a revision to the timeline.
Implementation date
I’ve noted some confusion in reporting and comments around ICD-11 approval by WHA and dissemination and implementation dates.
Unlike the U.S. specific ICD-10-CM, there is no mandatory date by which Member States must switch from using ICD-10 to ICD-11.
World Health Assembly adoption of ICD-11 and ICD-11 implementation dates are separate. WHA adoption enables official use for countries who wish to move on to the next edition. But Member States using ICD-10 will transition to the next version at their own convenience [6].
Once approved, prepared for implementation and released, global adoption of ICD-11 isn’t going to happen overnight. It may take several years before WHO Member States transition from ICD-10 to ICD-11. Low resource and developing countries may take longer to prepare for and transition to the new edition.
The annual update process for ICD-10 will continue during the creation of ICD-11.
Extracts from document [5] setting out the rationale and options for postponement of WHA Approval:
[…]
3. Progress and Current Status of ICD Revision:
[…]
BETA PHASE:
At this point in time, 1 September 2013, an ICD2013 Beta version has been produced for review purposes and field trials after 6 years of drafting phases.
The current ICD 2013 Beta version has relatively stable classification lists (i.e. linearizations) for Mortality and Morbidity recording. It will be reviewed by the specific Mortality Reference Group and the Morbidity Reference Group to see how well it fits the purpose and proposed transition from ICD‐10.
In addition, the Beta version has planned processes for:
(i) Systematic international scientific peer review (ii) Submission of additional proposals from public groups and scientists (iii) Conducting field trials for its applicability and reliability (iv) Production support in multiple languages (translations) starting with WHO official languages (v) Preparations for transitions from ICD‐10 to ICD‐11.
[…]
6. Timelines
The current ICD Revision Process timeline foresees that the ICD is submitted to the WHA in 2015 May and could then be implemented. Between now and 2015, there remains 20 months to conduct the remaining tasks summarized above as: 1. Reviews, 2. Additional Proposals, 3. Field Trials, 4. Translations, and 5. Transition Preparations.
Given the technical requirements these steps could be expedited in the next 20 months. The experience obtained thus far, however, suggests that this timeframe will be extremely tight for paying due diligence to the work especially in terms of: appropriate consultations with expert groups; communication and dissemination with stakeholders; and sufficient time for field testing in multiple countries and settings, and carrying out the resulting edits.
WHO Secretariat would like to discuss this with all stakeholders and evaluate the possible options:
a. Keep ICD submission to WHA to 2015 as originally planned and implementation / adoption date may be free by any Member State (current position – no change).
b. Postpone submission to WHA to a later year to allow longer time for field trials and other transition preparations.
[…]
In conclusion:
(a) WHO Secretariat could produce an ICD 2015 ready including Mortality and Morbidity Linearizations, Reference Guide and Index with the appropriate resolution to go to the World Health Assembly. This timeframe, however, is extremely tight for paying due diligence to the work especially in terms of: appropriate consultations with expert groups; and sufficient time for field testing in multiple countries and settings, and carrying out the resulting edits
(b) If the timeline is advanced to 2016, there will be more time to have ICD 2016 version with more translations and incorporations of some field tests results.
(c) If the timeline is advanced to 2017, ICD 2017 will be ready with most Field Test results incorporated and maintenance scheme tested.
[…]
Slide presentation: B Üstün, World Health Organization Classifications, Terminologies, Standards, ICD Revision: Quality Safety Meeting 2013 September 9-10
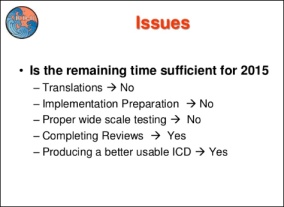
Where are we? What remains to be done? Shall we have ICD WHA submission in 2015 or later?
Slide 34:

Slide 35: [WHA Approval timeline – options under consideration]

References:
1. Newsletter on the WHO-FIC, Volume 11, Number 2, 2013, Latest News, Page 3. WHO Collaborating Centre for the Family of International Classifications (FIC) in the Netherlands.
2. IUPsyS Mar 08 Agenda Item 25 ICD-10 International Union of Psychological Science COMMITTEE ON INTERNATIONAL RELATIONS ACTION, March 28–30, 2008, Agenda Item No. 25: Revision of the International Classification of Diseases (ICD-10) and Involvement of Psychology.
3. Exhibit 1 WHO Letter Aug 07 Letter Saxena, WHO, to Ritchie, IUPsyS (International Union for Psychological Science), August 2007.
4. ICD-11 Timeline: http://www.who.int/classifications/icd/revision/timeline/en/index.html
5. Committee for the Coordination of Statistical Activities, Twenty-second Session 4-6 September 2013, Items for discussion and decision: Item 8 of the provisional agenda, 3 September 2013, Pages 8-10: http://unstats.un.org/unsd/accsub/2013docs-22nd/SA-2013-12-Add1-Health-WHO.pdf
6. Slide presentation: ICD Revision: Where are we? Bedirhan Üstün, World Health Organization Classifications, Terminologies, Standards, ICD Revision: Quality Safety Meeting 2013, September 9-10, 2013, Slides 29-35: http://www.slideshare.net/ustunb/icd-2013-qs-tag-260276686

Objectors to insertion of DSM-5’s Somatic symptom disorder into ICD-10-CM
November 16, 2013 by admindxrw
Post #283 Shortlink: http://wp.me/pKrrB-3y8
Michael Munoz, Executive Director, Rocky Mountain CFS/ME & FM Association has organized a joint letter of objection signed by 13 U.S. patient organizations and advocates for submission to NCHS. It can be read here:
http://www.rmcfa.org/index.html > http://www.rm-cfs-fms.citymaker.com/f/NCHS.pdf
or download PDF here: Joint response to NCHS 11.15.13
This joint submission had been signed by the following organizations and advocates:
I’d like to thank all those who have submitted objections to NCHS in opposition to the September 2013 C & M Committee meeting proposal to insert Somatic symptom disorder as an inclusion term in ICD-10-CM.
My submission can be read here PDF: Submission NCHS
Some additional organizations and individuals have advised me of their own submissions. If you have submitted a response on behalf of your organization or as a patient, advocate or professional and you would like your name or your organization’s name added to the list of responders below please shoot me an email or contact me via the Contact form with a link to your submission (if it has been placed in the public domain) and a couple of lines of credentials or stakeholder interest, if desired.
Share this:
Filed under American Psychiatric Association (APA), Darrel Regier, DSM-5, Functional Somatic Syndrome (FSS), ICD-10-CM, ICD-11, MUS, Myalgic encephalomyelitis, Somatic Symptom Disorder, Somatoform Disorders Tagged with american psychiatric association, dsm-5, functional somatic syndrome, icd-10-cm, icd-11, institute of psychiatry, NCHS, public comment, somatic symptom disorder, somatoform disorders