Between a Rock and a Hard Place: ICD-11 Beta draft: Definition added for “Bodily distress disorder”
January 29, 2014
Post #291 Shortlink: http://wp.me/pKrrB-3Gl
Update on February 2, 2014:
Since publishing my report, below, the Chapter 5 parent class:
“Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere”
has been reverted by ICD-11 Revision to read, “Bodily distress disorders”.
The category, 5C70 Psychological and behavioural factors associated with disorders or diseases classified elsewhere [F54 in ICD-10], which had been, and remains listed as an Exclusion to class “Bodily distress disorders”, is now coded towards the end of the list of Chapter 5 Mental and behavioural disorders categories, rather than listed as a hierarchical child category under:
“Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere”.
Note that the Definition and Inclusions for “5C70 Psychological and behavioural factors associated with disorders or diseases classified elsewhere” are legacy text carried over from ICD-10. The Fxx codes listed under “Exclusions” for this category have not yet been updated to reflect the new ICD-11 coding structure.
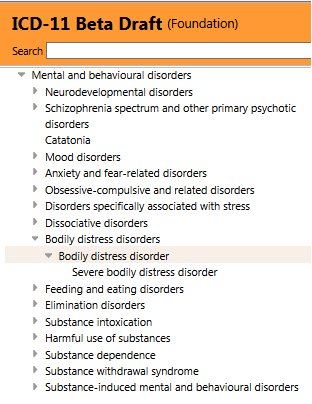
This section of Chapter 5 now displays as in this screenshot, immediately below, when viewed in the ICD-11 Beta drafting platform Foundation View, at February, 2, 2014:
A change also for Hypochondriasis – which has also been removed from under parent class, Bodily distress disorders, and is currently assigned dual parentage under: Obsessive-compulsive and related disorders; and Anxiety and fear-related disorders.
This means that the only categories currently coded under parent term “Bodily distress disorders” (previously, “Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere”) are “Bodily distress disorder” and “Severe bodily distress disorder“.
Update on February 1, 2014:
In June 2013, Prof David Goldberg co-authored a paper: Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (MUS) in Mental Health in Family Medicine. Co-author, Gabriel Ivbijaro, is Editor in Chief, Mental Health in Family Medicine and a past Chair of the Wonca Working Party on Mental Health. Mental Health in Family Medicine is the official journal of The World Organization of Family Doctors (Wonca) Working Party on Mental Health. I don’t have access to this paper, which is currently embargoed, but it should be free in PMC on June 1, 2014 [5].
Screenshot: Chapter 5, ICD-11 Beta drafting platform, public version: January 29, 2014
Between a Rock and a Hard Place
A definition for “Bodily distress disorder” has very recently been entered into the public version of the ICD-11 Beta drafting platform by ICD-11 Revision.
You can view the definition text, as it stands at January 29, in the public version of the Beta drafting platform, here:
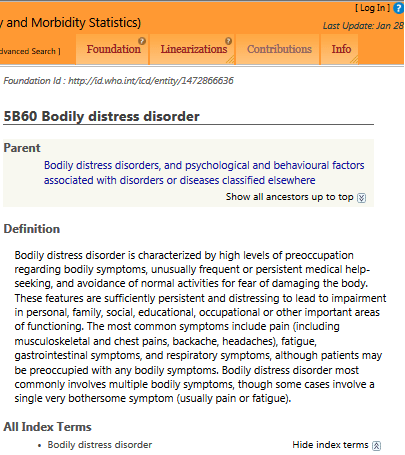
Joint Linearization for Mortality and Morbidity Statistics view
Bodily distress disorder
Parent(s)
Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere
Definition
Bodily distress disorder is characterized by high levels of preoccupation regarding bodily symptoms, unusually frequent or persistent medical help-seeking, and avoidance of normal activities for fear of damaging the body. These features are sufficiently persistent and distressing to lead to impairment in personal, family, social, educational, occupational or other important areas of functioning. The most common symptoms include pain (including musculoskeletal and chest pains, backache, headaches), fatigue, gastrointestinal symptoms, and respiratory symptoms, although patients may be preoccupied with any bodily symptoms. Bodily distress disorder most commonly involves multiple bodily symptoms, though some cases involve a single very bothersome symptom (usually pain or fatigue).
All Index Terms
- Bodily distress disorder
Or here, in the Beta Foundation view
—————-
Only the ICD-11 Short (100 word) Definition for this proposed new ICD category has been inserted. At this point, no Inclusion Terms, Exclusions, Synonyms, Narrower Terms, Diagnostic Criteria or other potential Content Model descriptors have been populated.
No Definition or severity characteristics have yet been assigned to Severe bodily distress disorder to differentiate between the two coded severities: “Bodily distress disorder” and “Severe bodily distress disorder.” (Unique codes for a “Mild bodily distress disorder” and a “Moderate bodily distress disorder” were dropped in mid 2013.)
In order to place this development into context here are some notes:
It’s important to understand that there are two working groups reporting to the International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders that are charged with making recommendations on the revision of the Somatoform Disorders for the primary care version and core version of ICD-11:
The 12 member Primary Care Consultation Group (PCCG) leads the development and field testing of the revision of all 28 mental and behavioural disorders for inclusion in the next ICD primary care classification (ICD-11-PHC), an abridged version of the core ICD classification. The PCCG is chaired by Prof Sir David Goldberg. Per Fink’s colleague, Marianne Rosendal, is a member of this group.
The 17 member Expert Working Group on Somatic Distress and Dissociative Disorders (S3DWG) is advising on the revision of ICD-10’s Somatoform Disorders. The S3DWG is chaired by Prof Oye Gureje. DSM-5 Somatic Symptom Disorder work group member, Prof Francis Creed, is a member of this group.
In 2011, the Primary Care Consultation Group’s proposals for a replacement for the “Unexplained somatic symptoms/medically unexplained symptoms” category were put out for review and evaluation in primary care settings to nine international focus groups* in seven countries [1].
*Austria, Brazil, Hong Kong, New Zealand, Pakistan, Tanzania and United Kingdom.
The PCCG anticipated refining their recommendations in the light of focus group responses before progressing to field testing the new disorder.
New disorders that survive the primary care field tests must have an equivalent disorder in the main ICD-11 classification.
Since any new primary care disorder concept will need to integrate into the ICD-11 core version, one might expect some cross-group collaboration between these two advisory committees.
But in their respective 2012 journal papers, the groups presented divergent constructs and neither group refers to the work being undertaken by the other group, or sets out how the two groups relate to each other, or how the primary care group relates to the overall revision process for the Somatoform Disorders.
The specific tasks of the S3DWG include, among others:
“3. To provide drafts of the content (e.g. definitions, descriptions, diagnostic guidelines) for somatic distress and dissociative disorder categories in line with the overall ICD revision requirements.
“4. To propose entities and descriptions that are needed for classification of somatic distress and dissociative disorders in different types of primary care settings, particularly in low- and middle-income countries.”
It is unclear how ICD-11 Revision is co-ordinating the input from the two groups, that is, will it be the PCCG’s revised recommendations that progress to field testing, this year, and if so, how would a divergent set of proposals, developed in parallel by the S3DWG group, relate to the field testing and to the overall revision of the SDs?
Or, will ICD-11 Revision require the PCCG group and the S3DWG group to agree on what to call any proposed, single disorder replacement for six or seven SD categories and to reach consensus over what construct, definition, characteristics and criteria will go forward to ICD-11 field testing, and if so, has consensus now been reached?
Field tests are expected to start this year. Currently, there is no publicly available information on the finalized characteristics, diagnostic guidelines, criteria, inclusions, exclusions, differential diagnoses etc. that are planned to be used for the field tests which would provide the level of detail lacking in this Beta draft definition.
It has been crafted with sufficient elasticity to allow either group’s construct to be shoehorned into it.
ICD-11 Revision is possibly hedging its bets depending on the outcome of its field tests. But the devil’s in the detail and without the detail, it isn’t clear whether this definition describes the construct favoured by the S3DWG in late 2012, or by the PCCG in mid 2012, or a more recent revision by one of the groups, or a compromise between the two.
The definition wording is based – in some places verbatim – on the construct descriptions presented in the Gureje, Creed (S3DWG) “Emerging themes…” paper, published in late 2012 [2].
Extract, Creed F, Gureje O. Emerging themes in the revision of the classification of somatoform disorders. Int Rev Psychiatry. 2012:
“…At the time of preparing this review, a major highlight of the proposals of the S3DWG for the revision of the ICD-10 somatoform disorders is that of subsuming all of the ICD-10 categories of F45.0 – F45.9 and F48.0 under a single category with a new name of ‘bodily distress disorder’ (BDD).
“In the proposal, BDD is defined as ‘A disorder characterized by high levels of preoccupation related to bodily symptoms or fear of having a physical illness with associated distress and impairment. The features include preoccupation with bothersome bodily symptoms and their significance, persistent fears of having or developing a serious illness or unreasonable conviction of having an undetected physical illness, unusually frequent or persistent medical help-seeking and avoidance of normal activities for fear of damaging the body. These features are sufficiently persistent and distressing to lead to impairment of functioning or frequent seeking of reassurance.'”
This 2012 paper goes on to say that the S3DWG’s emerging proposals specify a much simplified set of criteria for a diagnosis of Bodily distress disorder (BDD) that requires the presence of: 1. High levels of preoccupation with a persistent and bothersome bodily symptom or symptoms; or unreasonable fear, or conviction, of having an undetected physical illness; plus 2. The bodily symptom(s) or fears about illness are distressing and are associated with impairment of functioning.
And that in doing away with the “unreliable assumption of its causality” the diagnosis of BDD does not exclude the presence of depression or anxiety, or of a co-occurring physical health condition.
Which is a disorder construct into which DSM-5’s “Somatic Symptom Disorder” (SSD) could be integrated, thus facilitating harmonization between ICD-11 and DSM-5.
But without clarification from ICD-11 Revision (or further published papers, reports or sight of the field test protocol) I do not think one can safely extrapolate that it is the current proposals of the S3DWG group that are going forward to field testing, this year, in preference to a construct and criteria favoured by the PCCG group.
With the caveat that proposals by both groups are likely to have been modified since publication of their respective 2012 papers, or may have since converged into a consensus concept, to recap briefly:
In mid 2012, the Goldberg led PCCG primary care group was proposing a new term called “Bodily stress syndrome (BSS),” to replace ICD’s primary care category, “F45 Unexplained somatic symptoms.” This single BSS category would also absorb F48 Neurasthenia, which is proposed to be eliminated for ICD-11-PHC.
In late 2012, the S3DWG group was proposing to subsume the six ICD-10 categories F45.0 – F45.9, plus F48.0 Neurasthenia, under a single disorder category, but under the disorder name, “Bodily distress disorder” (BDD).
So at that point, the two groups differed on what term should be used for this new disorder.
The two group’s proposed constructs, criteria and exclusions also diverged, with the PCCG group incorporating characteristics of Fink et al’s “Bodily Distress Syndrome” [3] construct, and based on the “autonomic arousal” (or “over-arousal”) illness model, with symptom clusters or symptom patterns from one or more body systems, but also requiring some SSD-like psychobehavioural responses to meet the diagnosis. But, “If the symptoms are accounted for by a known physical disease this is not BSS.”
While the emerging proposals of the S3DWG group leaned more towards a “pure” DSM-5 SSD-like construct that could be diagnosed in patients with persistent “excessive” psychobehavioural responses to bodily symptoms in the presence of any diagnosed disease, patients with so-called “functional somatic syndromes” and patients with somatic symptoms of unclear etiology, but with no evident requirement for specific symptom counts, or for symptom clusters from one or more body systems or for the symptoms to be “medically unexplained.” [4]
What wasn’t explicitly set out in the PCCG’s 2012 paper was whether the group intended to mirror the Fink et al BDS construct to the extent of extending the diagnosis to be inclusive of the so-called “functional somatic syndromes,” FM, CFS and IBS (which are currently discretely coded or indexed within ICD-10 in chapters outside the mental and behavioural disorders chapter).
This 2013 paper, below, interprets that it is the intention of the Primary Care Consultation Group to capture FM, CFS and IBS:
http://www.ncbi.nlm.nih.gov/pubmed/24295235
Free PDF: http://www.uam.es/becarios/jbarrada/papers/hads.pdf
Psychol Assess. 2013 Dec 2. [Epub ahead of print] Bifactor Analysis and Construct Validity of the HADS: A Cross-Sectional and Longitudinal Study in Fibromyalgia Patients. Luciano JV, Barrada JR, Aguado J, Osma J, García-Campayo J.
“[…] In the upcoming primary healthcare version of the ICD-11 (ICD-11-PHC), FM will be classified as part of bodily stress syndrome (BSS; Lam et al., 2013). This new diagnosis will group patients who might have previously been considered different (e.g., those with FM, chronic fatigue syndrome, irritable bowel syndrome, and so on). Frontline clinicians (e.g., GPs) will need reliable tools to identify possible/probable clinical cases of anxiety (i.e., cognitive over-arousal) among patients with BSS who are characterised by elevated somatic over-arousal…”
Prof Tony Dowell, New Zealand, is a member of the PPCG. In this slide presentation Prof Dowell lists IBS, Fibromylagia and CFS under “Bodily Stress Syndromes.” Prof Dowell is already promoting the use of the BSS construct, in New Zealand, despite its current lack of validation:
Slide 29
Bodily Stress Syndromes
• Gastroenterology – IBS, Non ulcer dyspepsia
• Rheumatology – Fibromyalgia
• Cardiology – Non cardiac chest pain
• Respiratory – hyperventilation
• Dental – TMJ syndrome
• Neurology – ‘headache’
• Gynaecology – chronic pelvic pain
• Psychiatry – somatiform [sic] disorders
• Chronic fatigue Syndrome
Reading the responses of the focus groups, as reported in the Lam et al paper [1], it is evident that some focus group participants understood the proposed BSS construct as a diagnosis under which IBS, Fibromylagia and CFS patients could potentially be assigned; though one of the New Zealand focus groups noted there was quite a strong feeling that CFS did not fit the paradigm as well as other [FSS] disorders, particularly when there was a good history of preceding viral infection.
Whilst a number of diseases are listed in the PCCG criteria, as proposed in 2012, under “Differential diagnoses,” including multiple sclerosis, hyperparathyroidism, systemic lupus erythematosus and Lyme disease – IBS, Fibromylagia, CFS and ME are omitted from the list of “Differential diagnoses” examples.
In June 2013, Prof David Goldberg co-authored a paper: Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (MUS) in Mental Health in Family Medicine. Co-author, Gabriel Ivbijaro, is Editor in Chief, Mental Health in Family Medicine and a past Chair of the Wonca Working Party on Mental Health. Mental Health in Family Medicine is the official journal of The World Organization of Family Doctors (Wonca) Working Party on Mental Health.
I don’t have access to this paper, which is currently embargoed, but it should be free in PMC on June 1, 2014 [5].
—————-
When viewing the Beta drafting platform, note that the descriptive text for the ICD-11 Beta draft parent term, “Bodily distress disorders, and psychological and behavioural factors associated with disorders or diseases classified elsewhere,” which can be viewed here: ICD-11 Beta drafting platform Foundation view is the legacy text from the beginning of the ICD-10 Somatoform Disorders section (compare in ICD-10 here):
This F45 section introduction text has not yet been revised to reflect the proposed dismantling and reorganization of the ICD-10 Somatoform Disorders section for ICD-11.
Caveat: The ICD-11 Beta draft is not a static document – it is a work in progress, subject to daily revisions and refinements and to approval by the International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders, the ICD-11 Revision Steering Group, and WHO classification experts. Proposals for some new or revised disorders may be subject to re-evaluation and revision following ICD-11 field testing.
References:
1. Lam TP, Goldberg DP, Dowell AC, Fortes S, Mbatia JK, Minhas FA, Klinkman MS: Proposed new diagnoses of anxious depression and bodily stress syndrome in ICD-11-PHC: an international focus group study. Fam Pract Feb 2013 [Epub ahead of print July 2012]. http://www.ncbi.nlm.nih.gov/pubmed/22843638 [Full text behind paywall]
2. Creed F, Gureje O. Emerging themes in the revision of the classification of somatoform disorders. Int Rev Psychiatry. 2012 Dec;24(6):556-67. http://www.ncbi.nlm.nih.gov/pubmed/23244611 [Full text behind paywall]
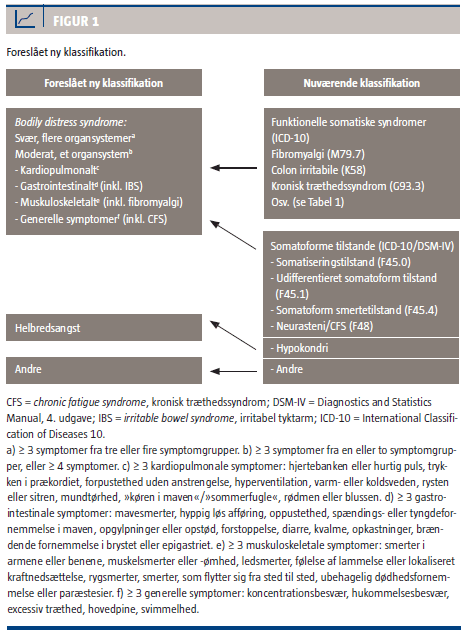
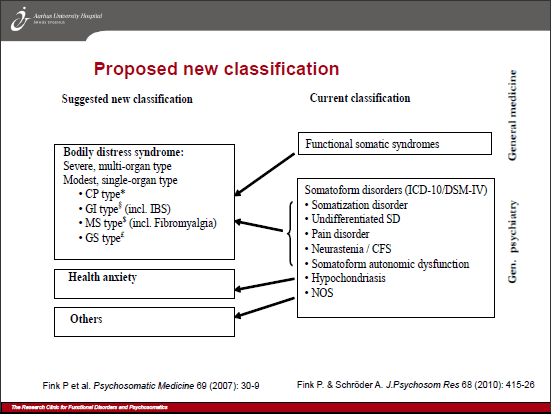
3. Fink et al’s Bodily Distress Syndrome
Per Fink and colleagues are lobbying for their “Bodily Distress Syndrome” (BDS) construct to be integrated into forthcoming classification systems and adopted as a diagnosis by primary care practitioners. They propose the reclassification of the somatoform disorders, pain disorder, neurasthenia and the so-called functional somatic syndromes, including fibromyalgia (FM), irritable bowel syndrome (IBS) and chronic fatigue syndrome (CFS), under a single, unifying diagnosis, “Bodily Distress Syndrome,” already in use in clinical and research settings in Denmark.
4. BDS, BDDs, BSS, BDD unscrambled
5. Ivbijaro G, Goldberg D. Bodily distress syndrome (BDS): the evolution from medically unexplained symptoms (MUS). Ment Health Fam Med. 2013 Jun;10(2):63-4. No abstract available. [PMID: 24427171] Currently embargoed: Free in PMC on June 1, 2014. PMC Archives
G Ivbijaro is Editor in Chief, Mental Health in Family Medicine and a past Chair of the Wonca Working Party on Mental Health. D Goldberg chairs the Primary Care Consultation Group (PCCG) leading the development and field testing of the next ICD primary care classification (ICD-11-PHC).
6. General information on ICD-11 Field Tests:
2012 Annual Report of the International Union of Psychological Science to the American Psychological Association Revision of World Health Organization’s ICD-10 Mental and Behavioural Disorders, Pierre L.-J. Ritchie, Ph.D, January, 2013, Pages 8-11
Click to access icd-report-2012.pdf
WHO ICD Revision Information Note: Field Trials, 23 January 2013
 2013 All rights reserved. Current Biology,
2013 All rights reserved. Current Biology, 
Keep SSD out of ICD-10-CM – November 15 deadline for objections
November 1, 2013 by admindxrw
Post #278 Shortlink: http://wp.me/pKrrB-3vK
Update: My submission on behalf of Dx Revision Watch can be read here.
The American Psychiatric Association (APA) has proposed the following DSM-5 disorders for inclusion in the forthcoming ICD-10-CM (Pages 32-44, September 2013 Diagnosis Agenda):
Additionally, APA has petitioned for revisions to the ICD-10-CM listing for gender dysphoria in adolescents and adults, which is not a new disorder.
On Page 45 and 46 of the Agenda, under Additional Tabular List Inclusion Terms for ICD-10-CM a number of other additions and changes to specific Chapter 5 F codes are being proposed, including the insertion of Somatic symptom disorder (SSD) and Illness anxiety disorder.
+++
A final reminder of the deadline for comments and objections in relation to Somatic symptom disorder
Q: When do objections need to be in by and where should they be sent?
A: Submit objections via email by November 15 to Donna Pickett, CDC: nchsicd9CM@cdc.gov
Q: Can anyone submit objections?
A: Yes. And from as many patient, professional and advocacy groups as possible, particularly from the U.S. but also international objections. Although this concerns potential changes to the draft of the U.S. specific ICD-10-CM there may be implications for ICD-11.
Q: What is being proposed?
A: The American Psychiatric Association has requested 6 new DSM-5 disorders for consideration for inclusion in the forthcoming ICD-10-CM via the September 18-19, 2013 ICD-9-CM Coordination and Maintenance Committee meeting.
APA’s rationales for these requested additions, the coding proposals and timings are set out on Pages 32 thru 44 of the September meeting Diagnosis Agenda.
But on Pages 45-46, under “Additional Tabular List Inclusion Terms for ICD-10-CM”, a further 17 proposals and changes are listed for consideration for addition to the Mental and behavioral disorders F codes.
These include the addition of the new DSM-5 categories, Somatic symptom disorder (SSD) and Illness anxiety disorder, as inclusion terms, under the ICD-10-CM Somatoform disorders section, thus:
Source: September 2013 Diagnosis Agenda, Page 45
The Diagnosis Agenda can be downloaded here: http://www.cdc.gov/nchs/data/icd/icd_topic_packet_sept_181913.pdf
Q: Is “Somatic symptom disorder” being proposed to replace several existing ICD-10-CM Somatoform disorders categories and is a unique new code proposed to be assigned to SSD?
A: No, not in the proposal as it stands in the Diagnosis Agenda document.
The proposal is to add SSD as an inclusion term under F45.1 Undifferentiated somatoform disorder. This is the ICD-10-CM code to which SSD is cross-walked in the DSM-5.
Illness anxiety disorder is being proposed as an inclusion term under F45.21 Hypochondriasis. This is the ICD-10-CM code to which Illness anxiety disorder is cross-walked in the DSM-5.
Q: What should I include in my objection?
A: Responders are being asked by NCHS/CMS to consider the following: Whether you agree with a proposal, disagree (and why), or have an alternative proposal to suggest.
Responders are also being asked to comment on the timing of those proposals that are being requested for approval for October 2014: Does a specific proposal for a new or changed Index entry and Tabular List entry meet the criteria for consideration for implementation during a partial code freeze [6] or should consideration for approval be deferred to October 2015?
And separately, and where applicable, comment on the creation of a specific new code for the condition effective from October 1, 2015. (This is not applicable in the case of SSD or Illness anxiety disorder.)
• Since no timing has been specified for the proposed insertion of the requests on Pages 45-46, I suggest stating that as a poorly validated disorder construct, SSD does not meet NCHS/CMS criteria for “new diseases/new technology procedures, and any minor revisions to correct reported errors in these classifications” and should not be considered for approval during a partial code freeze.
+++
On Day Two of the meeting, APA’s Darrel Regier presented 7 proposals for additions or changes, discussed APA’s rationales for each of these requests, in turn, and fielded any resulting questions or comments from the floor or from the meeting chairpersons.
Rationales, references, specific coding proposals for addition as inclusion terms in October 2014 (and subsequent code modifications in those cases where a unique new ICD code is proposed to be created for the term effective from October 2015) are also set out in the Agenda document (from Page 32).
But there was no presentation on behalf of APA, or by representatives of NCHS or CMS, or by anyone else for the specific proposal to add Somatic symptom disorder (SSD) and Illness anxiety disorder as inclusion terms under the ICD-10-CM Somatoform disorders.
No rationales for their inclusion or references to scientific evidence to support the validity of these new DSM-5 constructs have been published in the Diagnosis Agenda and there was no discussion of these two proposals during the course of the meeting.
The requesters of the proposals set out on Pages 45-46 are not identified, so it is unclear whether these “Additional Tabular List Inclusion Terms” are being proposed by APA or by NCHS/CMS.
• I suggest you comment in submissions on the absence from both the Agenda document and the meeting presentations of rationales and references to enable proper public scrutiny, consideration and informed responses to the proposed inclusion of these two terms.
All that was said about the list of proposals on Pages 45-46 was the following, after Dr Regier had wrapped up his own presentation and handed the podium back to the Co-Chair:
[Unofficial transcription from videocast] Donna Pickett (CDC):
• You might also consider quoting the APA’s disturbing DSM-5 field trial data (see March 2013 BMJ commentary by Prof Allen Frances for data).
• Or quote the SSD work group’s recognition of the shaky foundations and lack of scientific robustness for its new DSM-5 construct:
In its recent paper: Somatic Symptom Disorder: An important change in DSM, the SSD work group acknowledges the “small amount of validity data concerning SSD” and that much “remains to be determined” about the utility and reliability of the specific SSD criteria and its thresholds when applied in busy, general clinical practice, and there are “vital questions that must be answered.” [7]
• There is no body of published research on the epidemiology, clinical characteristics or treatment of the APA’s Somatic symptom disorder construct.
• There is a paucity of rigorous evidence for the validity, safety, reliability, acceptability and utility of the SSD construct when applied to adults and children in diverse clinical settings and across a spectrum of health and allied professionals.
• NCHS/CMS has insufficient scientific basis for the approval of SSD as a valid new disorder construct for inclusion within ICD; has published no independent field trial data and provided no rationale to inform public responses.
+++
Why is it important to submit objections?
If SSD is inserted as an inclusion term to an existing code in ICD-10-CM this may leverage the future replacement of several existing ICD-10-CM Somatoform disorders categories with the SSD construct, to more closely mirror DSM-5.
Inserting SSD as an inclusion term into ICD-10-CM may make it easier for ICD-11 to justify its proposal for a Bodily distress disorder to replace several existing ICD-10 Somatoform disorders categories. Though BDD may not mirror SSD exactly, it is anticipated to incorporate SSD’s characteristics and thereby facilitate harmonization between ICD-11 and DSM-5 disorder terminology.
As set out many times during the three DSM-5 stakeholder reviews and in several papers published earlier this year with Prof Allen Frances, DSM-5 SSD has highly subjective and loose, easily met criteria.
A mental health diagnosis of SSD can be applied as a “bolt-on” to any chronic medical diagnosis – to patients with cancer, diabetes, heart disease, MS, angina, ME and CFS, IBS, FM, chronic pain conditions. It can be applied to adults and children (or to the caregivers of children with chronic illnesses).
SSD may become the dustbin diagnosis into which those with persistent, “medically unexplained” somatic (bodily) symptoms will be shovelled. Patients with rare or hard to diagnose illnesses may find themselves mislabelled with SSD.
Implications for the potential impact on patients for an additional diagnosis of SSD are set out (about half way down the page) in my report Somatic Symptom Disorder could capture millions more under mental health diagnosis and in copies of submissions to the three DSM-5 stakeholder review periods, collated on this site.
Also in Mary Dimmock’s 2012 SSD Call to Action materials.
There is a now a copy of the 20 March, 2013 BMJ commentary “The new somatic symptom disorder in DSM-5 risks mislabeling many people as mentally ill” by Prof Allen Frances (with Suzy Chapman) on the NAPPS Skills (Northern Association for Persistent Physical Symptoms) site (Vincent Deary’s group) in this PDF.
If you’ve not already done so, please get an objection in before November 15.
And please alert all contacts, advocates, patient groups and professionals to the November 15 deadline and the need for input and objections.
Further information:
1 Crazy Like Us: How the U.S. Exports Its Models of Illness – DSM-5 is Americanizing the world’s understanding of the mind Christopher Lane, Ph.D. in Side Effects, October 9, 2013
2. Dx Revision Watch: APA petitions CMS for additions to ICD-10-CM: Deadline for public comment and objections November 15: http://wp.me/pKrrB-3tq
3. Dx Revision Watch: Videos and meeting materials: September 18- 19 ICD-9-CM Coordination and Maintenance Committee meeting: http://wp.me/pKrrB-3tV
4. Article: ICD Codes for Some DSM-5 Diagnoses Updated, Mark Moran, Psychiatric News, October 07, 2013:
http://psychnews.psychiatryonline.org/newsarticle.aspx?articleID=1757346
5. ICD-9-CM/PCS Coordination and Maintenance Committee Meeting September 18-19, 2013
September C & M meeting Diagnosis Agenda Proposals PDF document [PDF – 342 KB]
http://www.cdc.gov/nchs/data/icd/icd_topic_packet_sept_181913.pdf
6. Partial Freeze of Revisions to ICD-9-CM and ICD-10-CM/PCS
7. Somatic Symptom Disorder: An important change in DSM. Dimsdale JE, Creed F, Escobar J, Sharpe M, Wulsin L, Barsky A, Lee S, Irwin MR, Levenson J. J Psychosom Res. 2013 Sep;75(3):223-8. Epub 2013 Jul 25.
Share this:
Filed under American Psychiatric Association (APA), Bodily Distress Disorders, CMS, Criticism of DSM-V, DSM-5, Diagnostic classification, DSM-5, ICD-10-CM, ICD-11, Somatic Symptom Disorder, Somatoform Disorders Tagged with american psychiatric association, dsm-5, functional somatic syndrome, icd-10-cm, icd-11, institute of psychiatry, NCHS, public comment, somatic symptom disorder, somatoform disorders